 By Bob McNellis, M.P.H., P.A., AHRQ‘s Senior Advisor for Primary Care
By Bob McNellis, M.P.H., P.A., AHRQ‘s Senior Advisor for Primary Care
Twitter: @AHRQNews
The meeting took place nearly 15 years ago, but I still remember vividly the bold declaration by a former Congressional leader advocating for technological reforms in healthcare.
“Paper kills!” he warned. “Paper records are an utterly irrational national security risk.”
A few days earlier, the violent winds and rain of Hurricane Katrina had roared over the Gulf Coast. Flooding destroyed the health records of thousands of patients. Security concerns about paper-based records reached a fever pitch.
In some ways, it was a turning point. The anguishing loss of irreplaceable personal health care information turned what had been a murmur into a shout: No more delays — it was time for widespread use of electronic health records (EHRs).
Back then, as now, we understood that EHRs carried tremendous promise for improving care. Healthcare innovators envisioned a day when a primary care clinician had a patient’s latest medical history at his or her fingertips – the cardiologist’s most recent consult note, the immunizations given by the local pharmacist, a link to last month’s hospital discharge summary, and a real-time run-down of lab results. And, oh, by the way, notes from today’s visit would be sent to patients before they leave the office.
Calls for greater use of EHRs prompted a series of Federal incentive programs beginning in 2009. To date, these initiatives have provided over $37 billion in incentive payments to clinicians and hospitals to adopt health information technology, including EHRs. Since that meeting in 2005, use of EHRs in office-based practice has grown from about 24 percent to 86 percent in 2017. The growth of EHRs in hospitals is even more dramatic; in 2017, 96 percent of non-Federal acute care hospitals used an EHR.
Do these trends suggest we’re headed in the right direction? Definitely.
At the same time, are we struggling with obstacles to further success? Indeed, we are. And thanks to new data from AHRQ’s EvidenceNOW initiative, we understand more about the challenges of using EHRs among small to medium-sized primary care practices.
Launched in 2015, EvidenceNOW established regional cooperatives to support the delivery of evidence-based care and improve the heart health of patients at more than 1,500 primary care practices nationwide. Part of the effort has included ongoing health information technology support as well as evaluation of practices’ quality improvement efforts.
Here are some important findings from EvidenceNOW about the use of EHRs among small and medium-sized practices:
- EHRs are used by 93 percent of practices. We learned, however, that many of the EHRs these small and medium-sized primary care practices are using are not designed to support quality improvement or research.
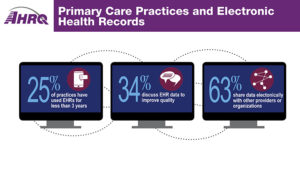
- Some practices are still new to their EHRs. About one in four practices have 3 or fewer years of experience with their current EHRs. Practices typically need ongoing support to navigate the learning curve, adjust their workflows, and improve efficiency.
- Most practices do report clinical quality measures to outside groups such as the Centers for Medicare & Medicaid Services (CMS) and private insurers, but few practices are using EHRs to report clinical quality measures. This represents a substantial missed opportunity to drive practice improvement.
- One-third of practices have never discussed their data as a team. Only 63 percent shared patient health data electronically with other providers or organizations.
- Practices often are unclear where to turn for technical assistance. Health information exchanges, hospital data networks, and clinical data warehouses can provide support, but these resources are not available to all practices.
An AHRQ infographic provides a snapshot of what we’ve learned about EHR use in small primary care practices. Clearly, challenges remain before we achieve our vision for effortless access to patient and population health data to help deliver evidence-based care and improve quality without increasing burden on clinicians and patients.
But the signs of progress are encouraging. The use of EHRs is nearly ubiquitous. We are making progress on interoperability, and thanks to new efforts by the Centers for Medicare & Medicaid Services and the Office of the National Coordinator for Health Information Technology, progress is likely to accelerate. It remains vital that we continue to identify, improve, and apply strategies that unleash the immense potential of EHRs to improve patient care.
This article was originally published on AHRQ Views Blog and is republished here with permission.
