 By Dana McCalley, VP of Value-Based Care, Navina
By Dana McCalley, VP of Value-Based Care, Navina
LinkedIn: Dana McCalley, MBA
LinkedIn: Navina
The shift from fee-for-service to value-based care (VBC) is a complicated one for any healthcare organization. It requires changes to workflows and processes across virtually all teams and oftentimes entails integrating new technologies to support them through this journey.
Engaging clinicians with value-based goals can be particularly challenging. They must maintain their commitment to delivering high-quality care while adapting to new value-based standards and requirements.
For the value-based model to work, the entire team needs to understand the ins and outs of VBC, the reasons behind the organizational shift, and how risk-based contracts impact how the practice brings in revenue.
Recognizing this need, clinician engagement’s importance is coming to the fore. Organizations taking on risk have found success in deploying the same tactics they use for pursuing their own value-based objectives to individual providers and teams to help drive organizational alignment.
Value-based care metrics to drive alignment
Just as risk-bearing healthcare providers are measured and reimbursed based on HEDIS measures and risk adjustment, many of these same metrics may be used–with some adaptation and simplification–to incentivize providers and drive their engagement.
For example, as a proxy for risk adjustment, organizations may choose to measure the rate at which providers document and account for Hierarchical Condition Categories (HCCs). In many organizations, those recommendations are created by pre-chart review teams. Such organizations can track the rate at which providers address the recommendations and document them in the chart.
Considering the wide variety of HEDIS measures, organizations may choose to measure clinicians on specific measures, based on areas where the organization sees greater opportunity to improve across the board. Such measures may include:
- Annual Wellness Visits
- 30-day readmission rates
- Order rates for screening procedures
Designing performance-based incentives
Just as healthcare organizations have had to adjust from receiving straightforward FFS reimbursement to variable reimbursements tied to shared savings, capitation, etc. those organizations who choose to incentivize providers must define frameworks for those incentives.
When designing incentivization frameworks, plans have a number of decisions to make, including:
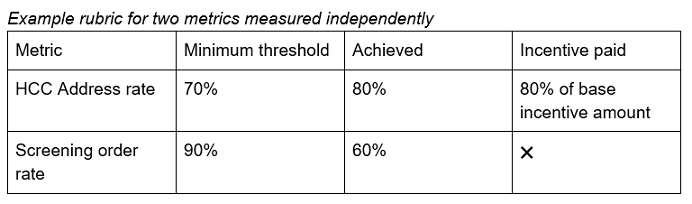
- Measuring performance on specific metrics individually or on overall performance across a group of metrics.
- Measuring individual providers on their performance independently, or distributing collective reward to teams or service lines.
- Granting incentives upon the achievement of certain minimum thresholds, or based on more granular percentile-based thresholds, where the payment will be a percentage of a base incentive amount.
Organizations considering incentive programs may elect to build financial compensation structures (for example, PMPM-based bonuses) around achieving certain results in the form of performance-based pay (i.e. separate bonuses or as part of the salary), or alternatively non-monetary rewards, such as personal time off.
Another important consideration is the time it takes organizations making the transition to VBC to see shared savings–often upwards of a year. If possible, organizations may prefer to pay incentive bonuses from the start of the transition process because of their direct contribution to its success.
Leveraging technology
While incentive models can be powerful motivators in shaping provider behavior, healthcare organizations must also ensure that their teams are equipped with the right technology to successfully enable them to meet their goals.
There are two key categories of tools organizations should consider when incentivizing providers on value-based care-oriented objectives.
- Tools that enable providers to achieve their goals better. For example, to drive improvement in HCC-related documentation, providers should be equipped with solutions that surface HCC recommendations in an accurate and trustworthy way at the point of care.
- Analytics tools that enable real-time performance tracking, for individuals to understand how they are performing at any given time.
Innovative AI solutions are especially well-suited to boost clinician engagement and alignment with value-based goals. By helping ease the administrative burden, these solutions can help enhance clinicians’ efforts and foster productivity and engagement.
Additionally, these tools are often an essential part of any incentive program as a means of measuring and providing analytics feedback on both individual and collective performance.
By arming physicians with innovative tools and thoughtfully designing and implementing incentive models, healthcare organizations can foster a culture that supports a quicker adoption of value-based care, leading to better care quality, provider satisfaction, and operational efficiency.
