 By Marty Callahan, President, Healthcare Markets, RevSpring
By Marty Callahan, President, Healthcare Markets, RevSpring
Twitter: @RevSpringInc
Healthcare CFOs’ priorities pull them in many directions:
- Cutting operational expenses
- Implementing innovative technologies
- Authorizing EHR upgrades
- Reviewing pricing contracts
- Improving revenue cycle efficiency
It’s easy to overlook quality of care as part of the financial equation with so many internal and external demands competing for a slice of your already limited budget. But ignoring quality metrics can have a detrimental effect on clinical outcomes, patient experience, and overall revenue streams in the long run.
We covered reasons why CFOs should focus on quality of care in a previous post, and now we will explore some of the financial and revenue cycle risks of ignoring quality metrics.
Risk #1: Declining Clinical Outcomes Measures
Why It Matters: Worsening clinical outcomes have a negative impact on reimbursement in value-based payment models.
The link between revenue cycle and clinical quality is only getting stronger as the scales continue to tip toward value-based payment models. If your health system can’t prove strong clinical outcomes, you’ll have a harder time collecting maximum reimbursements.
CFOs have a unique opportunity to impact clinical quality by building the IT infrastructure to support value-based care initiatives. Consider both proven and new technologies such as mobility solutions, blockchain, advanced analytics, and virtualization to improve workflows, provide access to accurate patient data, and achieve long-term cost savings.
Delaying technology investments will put your organization further behind the revenue cycle eight ball.
Risk #2: Bogging Down Employees With Heavier Workloads
Why It Matters: Freeing clinical and administrative staff from complex workflows and heavy workloads allows for happier patient interactions.
Health systems are service-based companies, so it’s important to cater to the needs and wellbeing of customer-facing employees. CFOs need to invest in technology that eases the loads on overworked staff — both clinical and administrative — to make them more available to interact with patients and provide exceptional care and service.
Many studies have shown a correlation between employee engagement and patient satisfaction. If patients and caregivers don’t feel the love from your entire team throughout their healthcare journey, they will take their business to a health system that offers coordinated patient engagement, billing communication, and care delivery across a connected enterprise.
Risk #3: Missing Opportunities to Be Innovative
Why It Matters: Evaluating technology and workflows with a quality of care lens will open your mind to solutions you wouldn’t have otherwise considered.
Patients want their healthcare experience to be more like their other consumer experiences, which means providers need to offer new, innovative ways to treat patients like valued customers.
A large component of bringing consumerism to healthcare is enabling multiple payment channels, including patient self-pay capabilities. As high-deductible health plans and rising out-of-pocket costs shift more of the financial responsibility from insurers to patients, convenience is king in the payment process.
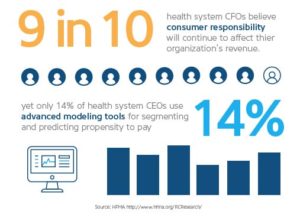
A 2017 HFMA survey found that 90 percent of CFOs and revenue cycle executives acknowledge that an increase in consumerresponsibility for the healthcare bill will impact their organization’s revenue, yet only 14 percent are investing in advanced modeling tools to predict patient propensity to pay, better understand their patients, and tailor billing options to improve financial outcomes.
In an interview with Becker’s Hospital Review at HFMA 2017, Sue Martin, SVP of Strategic Accounts at B. E. Smith, said in part, “Tools and processes related to price transparency, charity, and payment options are a must in today’s environment. Any time the patient payment process can be handled prior to care, the better. Build in proactive workflows and conversations toward making every visit about the care of the patient.”
A poor billing experience can sour even the greatest clinical encounter. If it’s not already, include the patient billing experience in your satisfaction surveys to keep a pulse on the quality of the entire patient experience before, during, and after the care encounter.
Balancing Quality and Costs
The CFO role involves more than number crunching and bottom line monitoring. Bringing compassion and care into the financial conversation will ensure CFO decisions are in the best interest of the patient and the health system.
Listen to your patients to understand how, when, and where they want to receive healthcare communications and manage healthcare payments so you can offer a more intuitive and seamless consumer experience.
This article was originally published on RevSpring and is republished here with permission.
