By John W. Loonsk, MD FACMI, CMIO CGI Federal and
Johns Hopkins Bloomberg Center for Population Health IT
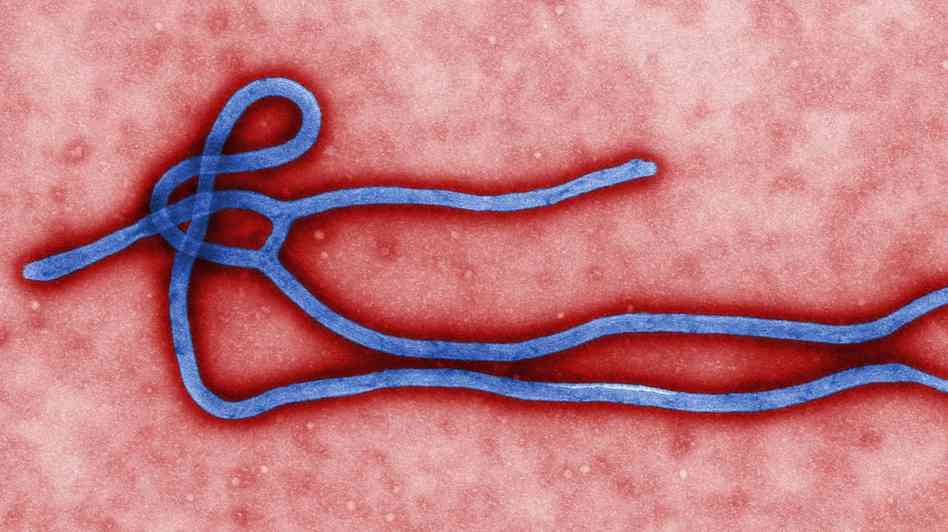
The Ebola cases in the United States, despite their limited numbers, have generated considerable discussion and anxiety. The discussion has included health IT because of the initial assertion that the Dallas hospital’s electronic health record led to the first US Ebola case being sent home. That claim was subsequently refuted, but it initiated conversation about whether the EHR was really to blame and, eventually, how EHRs might lean forward and help in such circumstances. Unfortunately, either way, the focus on EHRs in these Ebola discussions does not recognize more prominent outbreak health IT needs nor the ways we have yet to meet most of these needs with incentives and infrastructure.
Outbreak health IT and case reporting need attention too
The general outbreak anxiety is distressing and sometimes misplaced, but it does play an important role in motivating action. It is an unfortunate truth that emergency preparedness only gets attention during and shortly after emergency events. Work like health IT which requires sustained attention, incentives, standards, certification, and information exchange particularly suffers under these dynamics. An EHR did not cause the initial Ebola illnesses in the US, but health IT is also not yet aligned to substantially help with outbreaks either. Without adding to the anxiety, we should recognize the needs now and address them as soon as we can.
The health IT requirements for outbreak management and other public health emergencies are known (a list of such requirements is at the end of this article) and they are mostly not about EHRs. They do include health information exchange with EHRs but even this exchange, also known as “case reporting,” has not been addressed in HITECH incentive funds or Meaningful Use. And unlike clinical “continuity of care” health information exchange, there are no incentives in health reform to eventually accomplish it either. This is not health information exchange or interoperability that will be addressed by “market forces.”
As unfortunate as the situation is then, perhaps Ebola can break these dynamics, focus appropriate attention on some of these non-EHR aspects of health IT, and bring population health capabilities that can support outbreak management to the fore. These capabilities are needed for routine population heath purposes as well.
For now, EHRs should provide information and communication – not conclusions
The one possible role for EHRs right now is screening for additional cases now that an “index case” has already been identified in the US. This screening is important, but there are challenges to EHRs being effective in automating this use. There is also a large potential downside risk that next time an EHR would be appropriately blamed for a clinical misstep.
The effectiveness of EHRs for screening must be considered in the context of the level of provider awareness and changing guidelines. When provider awareness of the need to screen patients was low, EHRs could easily help raise awareness through casting a “wide net” and flagging patients for subsequent attention (high sensitivity). But now that provider awareness is high, the EHR “ask” looks more like the definitive adjudication of whether a patient should be a suspect case (high specificity). Unfortunately, among other issues, the recording and structure of travel history data is not strong in EHRs. The exposures of concern also continue to grow and change – first certain countries, then more countries, then exposure to health care workers who were exposed, then people on planes, ships and an expanding target.
All the while, the guidance that the Centers for Disease Control and Prevention are sharing is changing. This is not uncommon in outbreaks. There are legitimate reasons that guidance needs to be dynamic. But how do we know EHRs will represent the current state? Even when guidelines are stable, there are subtle issues in interpretation and implementation. What if the EHR gets it wrong? We know that clinical personnel at times ascribe definitive interpretation to guidance they get from computers. All of these factors suggest that EHRs right now should be used to provide information and facilitate communication and not to present “judgment.”
Outbreak management needs are much more than EHR interfaces
More broadly, the focus on this EHR screening role also distracts from the broader heath IT needs for outbreak management. Unfortunately, as in the Ebola discussion, the national health IT agenda continues to focus on EHRs. The Ebola events come into harsh contrast with the most current health IT focus on interfaces with EHRs (also called APIs – Application Programming Interfaces). EHR APIs were by no means the only suggestion of the recent JASON review and report, but they are what seems to be an almost singular focus of the response. Outbreak management, connecting lab results and case data, contact tracing and other functions have requirements that don’t relate to EHR APIs. Health IT architecture in the US must consider broader needs too.
Much of what needs to be done for outbreak management health IT will not be done in the immediate months of this Ebola crisis. It is critically important, though, that we note the broad needs now and commit to addressing them as soon as we can. Hopefully Ebola will not fully demonstrate their importance, but already Ebola has shown some of these needs.
Outbreak management health IT needs
Part of what makes outbreak management health IT challenging is that outbreaks and public health emergencies are highly variable. Nature and its diseases are themselves variable, but when one maps these diseases across complicated global and national infrastructure and organizations, there are many different ways that events can play out. Ebola hopefully will stay at low case counts in the US and thus not require all of this health IT infrastructure. But if not, or during the next event, any of these needs could be made prominent.
There are functional needs for outbreaks and known technical approaches for addressing them. Outbreak health IT infrastructure needs to largely be in place and in use before emergency events (it is hard to build, train and deploy infrastructure on the fly), but the in-place infrastructure also needs to be flexible enough to support variations in the way that different outbreaks and public health emergencies proceed.
In-line with their usual progression, here are some outbreak needs that are shared in part by the Ebola, Anthrax, SARS, MonkeyPox and other emergency events and some conclusions about their health IT support:
- “Index” case detection: A lot of academic effort and public money for syndromic surveillance has gone into trying to get health IT to help identify the first case of something before it is apparent to health care providers. For the current Ebola situation in the US, the first Dallas case would be the “US index case.” For a brief period of time before that case appeared, but while there was public health awareness of the outbreak in Africa, having an EHR algorithm that focused on travel history or exposure and influenza-like symptoms might have raised clinical awareness of the circumstance and helped prevent some of the Dallas events. It is not an EHR “issue” that EHRs did not have this, but it is a way that the EHR could have possibly helped. But definitive clinical decision support for low-specificity index case detection is challenging because of vague symptomology and narrative patient history characteristics. The specific operative data are not consistent across EHRs. There are also no standards for distributing decision support algorithms. With the subsequent variations in implementation for decision support in the real world there is then also the strong possibility of automating solutions that produce incorrect answers.
Analysis
Decision support for “index case” detection is still experimental, hard to implement in EHRs, and should not distract from the established and substantive health IT needs of outbreak management.
- “Screening” and Subsequent Case Detection: It is important to differentiate the situation following the identification of an index case – where we are now for Ebola – when clinical awareness has already been elevated. The issue then for clinical personnel is not about alerting them to pay attention – they are. It is more about helping them make decisions about borderline “suspect” cases. Unfortunately, in addition to the travel history issues expressed above, fever and other influenza-like symptoms that Ebola presents with are commonplace and non-specific. We are, after all, going into flu season.
As things progressed for US cases it has rapidly reached a point where anyone with any exposure history who presents for care needs some degree of consideration. Well-trained clinical care personnel who reach out to public health are going to be the best “screeners” for some time to come.
Analysis
By all means implement “wide-net” provision of guidance and methods of follow-up, but don’t overemphasize the automation of whether a patient is a suspect case or not – first do no harm. Recognize the limits of the role EHRs play here and focus more on critical non-EHR health IT.
- Case Reporting: Electronic data on suspect cases, confirmed cases and ancillary case data need to be delivered to other electronic systems than EHRs. EHRs are designed to support the provision of care and there are many needs in these circumstances that EHRs don’t begin to address. Data on these cases need to be provided for management in an outbreak context; to record contacts with other people and exposures, to manage their status from suspect through elimination or confirmation, to monitor the spread of disease at many different population levels and to set-up next steps of action for isolation, countermeasure administration or just policy development and research.
At low case levels, like those currently for Ebola in the US, the number of suspect cases coming from EHRs is low. Electronic case reporting from EHRs to outbreak management systems becomes even more important as rates increase. The syndromic surveillance that is in Meaningful Use does not address this critical need. Public health has approaches for automated case reporting that don’t require significant effort from EHR vendors or clinical care providers but they are not currently being implemented.
Analysis
Case reporting from EHRs to public health should be a top priority for Meaningful Use. Funds should also be provided to public health to support their side of this data exchange.
- Case management: When a possible case has been identified (sent from an EHR or received from an airplane manifest or other source) it needs to be received and then managed by a surveillance system that supports outbreak management. Robust and standards-based systems that can accept standards-based case exchange should be available and certified to cover every jurisdiction in the US. There have been numerous exercises that have demonstrated these needs, but always limited funding to implement them. These systems need to be able to link case data with lab results that confirm or refute suspect cases and support other functions. There are both management and analytic needs here and both needs must be considered in the context of data exchange and functionality.
Analysis
Certification of public health systems to ensure interoperability is needed. Just as in e-prescribing, when the non-EHR system involves more than just data analysis, there is a critical need to have a reliable, active and well-tested connection to it.
- Contact tracing: Ebola has elevated attention to the process of “contact tracing.” Surveillance systems that support outbreak management need to record the exposures that cases and possible cases have so these contacts can be monitored for the disease. This is a key public health process where IT systems are very helpful. Even when there are low counts for suspect cases, the number of possible contacts can be large. When those contacts start to be confirmed as cases, the contacts of the contacts become a consideration and the math can progress geometrically. Interoperable electronic systems are critical for this management. When SARS hit Toronto, and that more communicable disease had a substantial foothold, it was suppressed though the application of just such computerized processes. US preparedness requires knowing the coverage of interoperable health IT systems to support contact tracing. It also needs public health professionals trained in the use of these systems when they do exist.
Analysis
Measure and track the functionality of public health systems as well as EHRs. Implement training and routine use of appropriate systems before emergency events and ensure that personnel are certified in their use.
- Countermeasure Administration: An Ebola vaccine is very desirable and would obviate many of the aforementioned health IT needs. There is a temptation, however, to think that in a big emergency, vaccines and pills would be distributed freely. In practice, however, real world examples and disaster scenarios have shown that here too there are needs for systems to track and manage an outbreak response. When a vaccine comes available, it will only be available in limited supply. At that stage, there is a need to coordinate vaccine administration with the possible cases and other potential contacts to support a “ring vaccination” strategy. Experience from the Smallpox vaccination program has also shown that there are frequently heightened needs to monitor the recipients of early vaccines for side effects and efficacy. Connection of surveillance systems to vaccine delivery systems is needed for this type of surveillance as well. Finally, isolation is another countermeasure. Systems need to manage and track possible contacts that need to be isolated or quarantined whether that is in their homes or elsewhere.
Analysis
Interoperable countermeasure administration systems should be supported, certified, tested, and available to support several different levels of available vaccines, drugs and other countermeasures.
- Research: The Ebola response has already shown how many things are not known about the spread and management of even this well-established disease. Getting consistently recorded data during and after the event is important to learn how to better handle a recurrence and other public health emergencies. Most of these data will not come from randomized controlled trials, but from real world experiences that are then transmitted to longer term registries. Most of the research work occurs after the crisis is over, but the data need to be considered during the event.
Analysis
Interoperable EHRs and other systems need to share data appropriately with research-related systems to best learn from emergency events and plan future responses.
This article was originally published on Government HealthIT and is republished here with permission.
