 By Angela Jordan, Senior CDI Consultant, abeo
By Angela Jordan, Senior CDI Consultant, abeo
Twitter: @abeoManagement
The Transitional Care Management (TCM) codes (99495, 99496) introduced in 2013 allow providers to report and capture reimbursement for the work involved with providing continuity of care to patients discharged from a hospital or other qualified stay, back into their community setting. Unlike new and established evaluation and management codes, the TCM service spans 30 days. The components take into account the work of the provider and the work of their clinical staff.
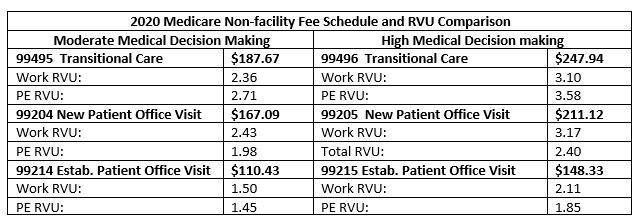
Those that haven’t instituted a TCM program are quite possibly missing out on additional revenue. When you compare the Medicare reimbursement for office evaluation and management services to TCM using the 2020 National Medicare Fee schedule, you can see the reimbursement is higher due to the additional relative value units (RVUs) for practice expense. This is compensating the practice for the additional activities provided during the 30 period by your clinical and ancillary staff.
However, be careful. Don’t start reporting TCM services without understanding all of the rules and documentation requirements. Every patient that is discharged from a qualified stay will not meet the requirement to report the service. Only those patients that require moderate to high medical decision making can be considered for transitional management. Review the codes and descriptions in AMA CPT@ 2020 edition.
*99495 – Transitional Care Management Services with the following required elements:
- Communication (direct contact, telephone, electronic) with the patient and/or caregiver within 2 business days of discharge
- Medical decision making of at least moderate complexity during the service period
- Face-to-face visit, within 14 calendar days of discharge
*99496 -Transitional Care Management Services with the following required elements:
- Communication (direct contact, telephone, electronic) with the patient and/or caregiver within 2 business days of discharge
- Medical decision making of high complexity during the service period
- Face-to-face visit, within 7 calendar days of discharge
Below is a list of requirements in addition to the face-to-face and non-face-to-face services that are expected and should be documented in the patient’s record for the 30-day period:
- Patient must be discharged from an inpatient hospital setting (acute hospital, rehabilitation hospital, long-term acute care hospital), partial hospital, observation status in a hospital, or skilled nursing facility/nursing facility. (Emergency department discharge does not qualify)
- Patient must be discharged to their community setting, home, domiciliary, rest home or assisted living.
- TCM starts the day of discharge and continues for the next 29 days.
- There must be interactive contact with the patient or their caregiver within two business days of the discharge.
- Discharge medications must be reconciled before or during the face-to-face visit.
- The face-to-face visit must be made within 14 calendar days of the discharge.
- Medical decision making must be moderate or high during the service period.
- Some Medicare Administrative Contractors (MAC) indicate the medical decision making is determined at the face-to-face visit.
- Non-face-to-face services by the physician or other qualified health care provider:
- Obtaining and reviewing the discharge information
- Reviewing the need for or follow-up on pending diagnostic tests and treatments
- Interaction with other qualified health care professionals who will assume or reassume care of the patient’s system-specific problems
- Education of patient, family, guardian, and/or caregiver
- Establishment or reestablishment of referrals and arranging for needed community resources
- Assistance in scheduling any required follow-up with community providers and services
- Non-face-to-face services by clinical staff:
- Communication (with patient, family members, guardian or caretaker, surrogate decision makers, and/or other professionals) regarding aspects of care
- Communication with home health agencies and other community services utilized by the patient
- Patient and/or family/caretaker education to support self-management, independent living, and activities of daily living
- Assessment and support for treatment regimen adherence and medication management
- Identification of available community and health resources
- Facilitating access to care and services needed by the patient and/or family
Important note, TCM can be provided as a telemedicine service, as noted by the * in CPT@. When telemedicine is used, the best practice is to document the platform used and that the visit utilized audio and video, and the patient agreed to the visit. It would also be beneficial to note if the system used is HIPAA compliant.
With the 2021 changes to Office and Other Outpatient Services (99202-99215), there have been questions regarding the use of the new “CPT E/M Office Revisions Level of Medical Decision Making (MDM)” table. At this time, the instructions in CPT for 2021 direct you to the MDM instructions for the “E/M Services Guidelines,” which are currently used.
Transitional care management is just one area where your organization could be missing out on reimbursement. Whether its for identifying areas of missed revenue, improving standardization methodologies or improving coding accuracy for less compliance risk, organizations should make sure they are always performing internal coding audits, along with the occasional professional assessment as well.
