
By Terry Edwards, President and CEO, PerfectServe
Twitter: @perfectserveCEO
Twitter: @PerfectServe
Since the era of meaningful use began more than five years ago, healthcare providers have made great strides in implementing electronic health records (EHRs) within their facilities. The EHR market is now in the billions of dollars annually in the U.S. alone, and HealthIT.gov estimates that $22.5 billion in incentives will be paid to providers for adoption of EHR technology between the years of 2011-2022.
While the goals of the EHR are laudable – contributing to more accurate and complete digital patient records, better coordinated care across providers and care settings, and improved patient engagement – a recent survey shows that EHRs have fallen short of expectations. The survey, which polled 955 healthcare professionals[1], was conducted online by Harris Poll and commissioned by PerfectServe.
The survey revealed that only 60% of healthcare professionals surveyed believe the EHR is sufficient for care coordination and collaboration across the healthcare continuum: clinicians[2] (53%) are less likely to agree with this than nurses (69%) and office managers/practice administrators (69%*).
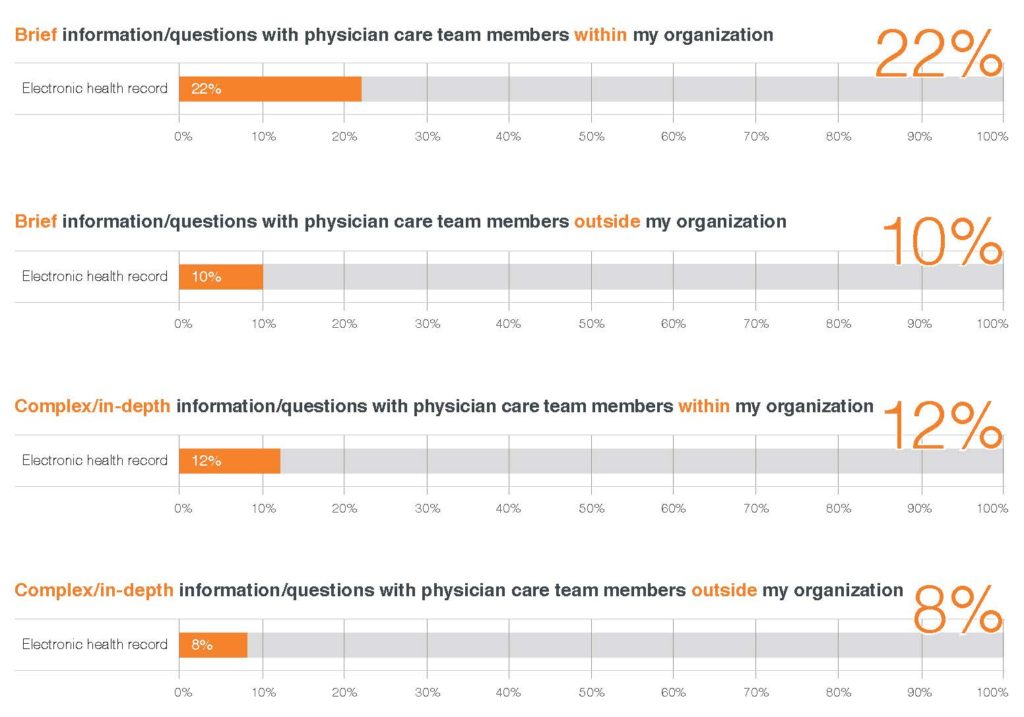
The survey also indicates that when the complexity of the information increases, the usage of the EHR for communication decreases. When sharing complex, detailed information with physicians outside of their organization (for example, with primary care physicians (PCPs) and specialists), only 8% say the EHR is their primary method of communication.
 With all the time and money invested in this technology, how can this be? The following causes may play a role:
With all the time and money invested in this technology, how can this be? The following causes may play a role:
- Reliance on older communication technologies – In this study, most healthcare professionals surveyed (62%) say phone calls are the most frequently used method when communicating complex or in-depth information with physicians outside their organization. Is this because there is a need for providers to talk with each other in real time? Or is this as a “chicken and egg” situation, e.g. – the less we use the EHR to communicate, the less valuable it appears, which then further limits the perception of its usefulness?
- A lack of interoperability between systems – The lack of interoperability between healthcare IT systems is a continuing challenge, making it hard for the EHR to live up to its expectations.
- EHR inflexibility and lack of acceptance – According to the National Institute of Standards and Technology (NIST)[3], clinicians often have to adapt their workflows to the EHR system, rather than the other way around, leading to a decrease in productivity. This leads to a lack of acceptance of the EHR system, a low perception of its value and a tendency to record the least possible information to get by.
- Heavy footprint – The EHR is a pretty heavy application that, for many, is best accessed via a computer with a big monitor. It’s just too big and heavy for quick, provider to provider communication that is often role based. The EHR just does not know who is in what role at every moment in time.
Time may heal some of these shortcomings. The next generation of clinicians is sure to be more comfortable with the use of modern communication technologies in the workplace. EHR vendors will hopefully continue to evolve their systems to improve user experience, and providers may be able to apply enough pressure to vendors to address the interoperability challenge in a meaningful way. Over time, EHR utility and acceptance will rise.
However, I believe the best prescription for the EHR issue today is to use the EHR system for what it does best – acting as a repository of clinical information, a “system of record,” to simplify accessing patient data. If we do that, and implement comprehensive and secure communication and collaboration solutions in parallel, we can have the best of both worlds – a reference point for clinical information and a better, more timely way to make the right people aware of and share pertinent information with members of the extended care team.
About the Survey
The PerfectServe survey was conducted online by Harris Poll on behalf of PerfectServe between February 12 and March 6, 2015. The research was conducted among 955 healthcare professionals in the following occupations: hospitalist (n=150), primary care physician in an office (n=150), specialist physician in a hospital (n=102), specialist physician in an office (n=101), hospital administrator (n=170), office manager/practice administrator (n=81), nurse in a hospital (n=101), and case manager (n=100). Office-based respondents work in an office with 25 or more physicians.[4] Hospital-based respondents work in a hospital with 200 or more beds. Physician respondents are duly licensed in the state in which they practice. Data were not weighted and are only representative of those who completed the survey.
*low base size; results should be interpreted as directional in nature
[1] Polled healthcare professionals include: hospitalists, primary care physicians in large offices, specialists in both hospital and office settings, nurses in hospitals, case managers, hospital administrators and office managers
[2] “Clinicians” includes all physician categories surveyed, nurses and case managers, and excludes hospital administrators and office managers.
[3] Svetlana L.Z, Patterson E.S, et al. “Integrating Electronic Health Recordsinto Clinical Workflow: An Application of Human Factors Modeling Methods to Ambulatory Care”, National Institute of Standards and Technology, 2014.
[4] 9 Office Managers/Practice Administrators work in an office with fewer than 25 physicians.
About the Author: Terry Edwards is the visionary founder, president and CEO of PerfectServe. As chief executive, Edwards has dedicated himself to helping clinicians provide the best and most efficient patient care—while delivering most satisfying customer experience in the healthcare industry. This article was originally published on The Connected Clinician and is republished here with permission.
