Sepsis Detection in Acute Care: Key Insights from Our Sepsis Alliance Webinar
Prenosis recently presented a webinar with the Sepsis Alliance Institute, examining how advanced biomarker analysis improves sepsis detection and diagnosis. The presentation – led by Prenosis’ Robin Carver, former bedside nurse, and Jim Sianis, former clinical pharmacist – highlighted the significance of Prenosis’ personalized approach to this critical condition.
The Clinical Challenge of Sepsis Detection
The clinical burden is substantial: 1.7 million patients develop sepsis annually in the U.S., resulting in over 350,000 deaths. Hospitals experience an average loss of $29,118 per septic patient. There is no definitive diagnostic test for sepsis; clinicians must rely on a combination of early warning systems, various point-of-care tests, and clinical judgment while managing the risk of rapid progression to severe sepsis.
Current diagnostic tools, while important, cannot address the inherent heterogeneity of sepsis. As Robin noted from her experience as an ED triage nurse, patients present with everything from toothaches to severe infections they’ve been self-treating for days. “Patients are sicker when they walk in and ultimately at risk for deterioration faster,” she explained.
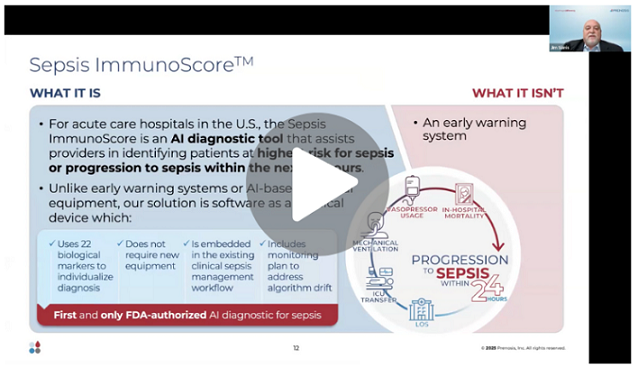
To tackle this variability, Prenosis developed Sepsis ImmunoScore™ – an AI diagnostic tool that provides clinicians with an objective, patient-specific risk assessment.
Evidence-Based Approach to Clinical AI Implementation
There are three fundamental requirements for clinical adoption of AI diagnostic tools:
- Comprehensive external validation
- Transparent algorithmic methodology
- Ongoing performance assessment
Prenosis’ development process for Sepsis ImmunoScore involved creating a robust, longitudinal biobank from 11 hospital sites, paired with detailed clinical data. This evidence-based approach enabled analysis of individual immunological responses to infection and development of the diagnostic algorithm.
Prenosis pursued the De Novo regulatory pathway with the Food & Drug Administration (FDA). Sepsis ImmunoScore™ is the first FDA-authorized AI diagnostic for sepsis, providing clinicians with an objective assessment of patients at elevated risk for sepsis or progression within 24 hours, based on 22 biological markers.
Clinical Workflow Integration
A critical factor in clinical adoption is seamless integration with existing workflows. As Robin emphasized, “Many promising technologies fail because they disrupt rather than integrate into existing clinical workflows.” The Prenosis solution is EMR-agnostic and designed to complement current sepsis protocols. The system can be configured to order Sepsis ImmunoScore upon early warning system activation or be directly ordered through the EMR, providing an additional layer of objective data before treatment decisions.
Patient-Specific Risk Assessment
To demonstrate clinical utility, the webinar included a comparison of two patients. While one patient appeared healthy with slightly low blood pressure and elevated temperature, another patient presented with a more complicated medical history and concerning heart rate. Traditional assessment would likely send the first patient home with antibiotics and the second patient to be admitted to the hospital.
However, as Jim explained, “The Sepsis ImmunoScore validates that the individual parameters that drive a patient’s risk vary from individual to individual – demonstrating the heterogeneity of these patients. This is what enables us to ‘see people differently.’”
SEP-1 Compliance and Evolving Evidence
Recent publications have questioned the impact of CMS sepsis bundle compliance on mortality benefits. Despite studies in JAMA and Annals of Internal Medicine that indicate limited mortality improvements, Robin acknowledged that “SEP-1 remains embedded in CMS Value-Based Purchasing, affecting reimbursement and hospital ratings.” While standardizing care and accelerating interventions like antibiotic timing, there remains a need for more effective patient classification.
A 2024 analysis of Prenosis research data demonstrated that implementation of Sepsis ImmunoScore™ could reduce antibiotic overprescription by 40% while identifying 73% of SEP-1 bundle non-compliance cases.
This article was originally published on the Prenosis blog and is republished here with permission.