 By Christian Kratsas, Content Marketing Specialist, Treatspace
By Christian Kratsas, Content Marketing Specialist, Treatspace
Twitter: @Treatspace
Patient Centered Medical Home (PCMH) embodies the current trajectory of healthcare in that the patient is the focus of the medical model. The National Committee for Quality Assurance’s (NCQA) PCMH program is vastly adopted, with more than 12,000 practices, 60,000 clinicians, and 100 payors participating. In fact, 1 in 6 eligible physicians in the U.S. practices in an NCQA-Recognized PCMH.
With the objective to strengthen patient-provider relationships, reduce healthcare costs, and improve quality, NCQA continues to accelerate the growth of value-based care with the remodel of their PCMH program. Changes to the new PCMH model reduces the burden of the reporting process and focuses on increased healthcare quality and practice performance.
Redesigned reporting process and criteria
The redesigned PCMH program is effective September 30th, 2017 and practices that plan to get recognition using the 2014 standards must do so before then. Most notably, “once the practice has been recognized as a medical home, it will never have to renew its application from start to finish,” explained Michael Barr, MD—executive vice president of the organization’s quality measurement and research group—in a recent Medical Economics article detailing the changes.
In addition to the ongoing recognition status, reporting is moving from a three-year cycle to an annual online “check-in” with a dedicated NCQA point of contact. Fortunately, screenshots and egregious written documentation is reduced in the new redesign. Online interaction, facilitated through a screen-sharing session, and data submission is now the method that practices employ to prove they are meeting core requirements.
Out of the 17% of primary care practices in the U.S. that wield NCQA’s PCMH badge, 75% of them are recognized as PCMH level 3. To demonstrate the majority of level 3 practices, the new recognition structure is flattened to a single level. Vice President of Product Design and Support, Patricia Barrett explains that the change will enable “a much clearer delineation between practices that are recognized by the NCQA and those that aren’t.”
Increased patient satisfaction and financial reward
The origin of practice transformation for many medical homes revolves around highly collaborative provider relationships for improved patient care.
According to a Hartford Foundation Study, 83% of patients said that being treated in a PCMH improved their health¹.
In addition to improved health, patients are more satisfied with urgent appointment scheduling. In a study published in Becker’s Hospital review, patient satisfaction increased from 12 percent to 53 percent in a PCMH practice, while in the control clinics the scores improved from 14 percent to 18 percent.
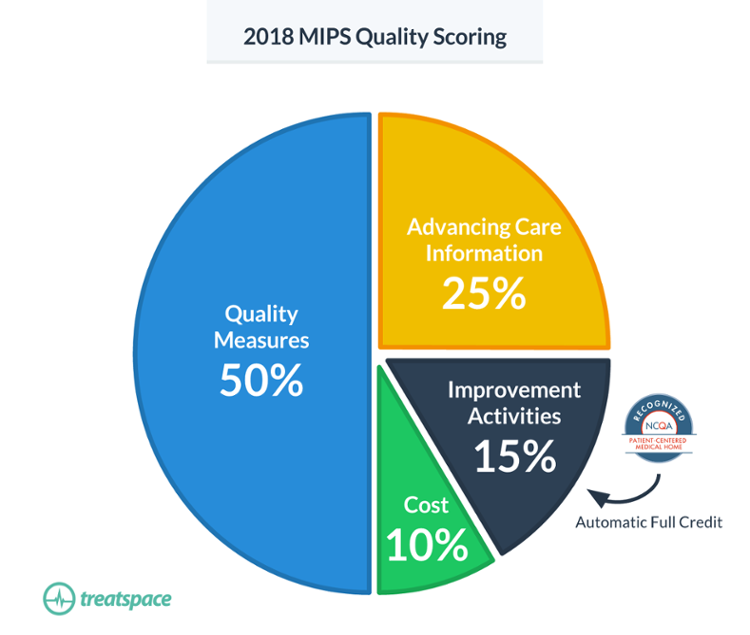
Redesigned PCMH guidelines are preparing practices for prospective models of payment that incentivize patient-centered care. According to the NCQA Toolkit, available for download on their website, “becoming an NCQA-Recognized PCMH or PCSP directly increases clinician payments through the Merit-Based Incentive Payment System (MIPS).” Improvement Activities account for 20% of a practice’s MIPS score (15% in 2018) under MACRA and as a NCQA-Recognized PCMH or PCSP that practice will receive automatic full credit in the category.
“…becoming an NCQA-Recognized PCMH or PCSP directly increases clinician payments through the Merit-Based Incentive Payment System (MIPS).”
The other 3 categories contributing to MIPS; Quality Measures, Advancing Care Information, and Cost (2018), will likely be met by PCMH practices. Measures set forth in the recognition program that improve coordination of care, promote the use of health information technology (HIT), and improve patient outcomes overlap with MIPS requirements.
Finally, more than 100 payors are offering financial incentives to practices operating within the PCMH framework. Accredited practices must “seek out value-based contracts to fully capitalize on the transformation,” as encouraged by MGMA. In the same article, Steven Blubaugh of DHG Healthcare explains that practices “risk missing out on very important revenue by not asking commercial payers to increase their reimbursement due to improved care delivery.”
¹ Hartford Foundation | Transforming Primary Care What Medicare Beneficiaries Want and Need from Patient-Centered Medical Homes to Improve Health and Lower Cost
This article was originally published on Treatspace and is republished here with permission.
