 By Arun Rangamani, SVP, Analytics & Technology, SCIO Health Analytics
By Arun Rangamani, SVP, Analytics & Technology, SCIO Health Analytics
Twitter: @SCIOanalytics
Healthcare business intelligence and analytics today needs to be faster, more comprehensive and more insightful than ever before. It’s a tall order that is proving to be too much for current business intelligence models (see “Current Models No Longer Making the Grade”). Emerging business intelligence PODs – or cross-functional and multidisciplinary teams that bring together design and engineering to deliver the optimal results – could come to the rescue and eventually take hold as the new centers of excellence (CoE) that will deliver much needed value in these demanding times.
Instead of approaching business intelligence with teams composed of homogenous staff members, the POD teams will consist of a diverse array of staff members such as data scientists/statisticians, big data engineers, clinical staff, healthcare coding experts, application developers, visualization experts, tech writers and technology enablers.
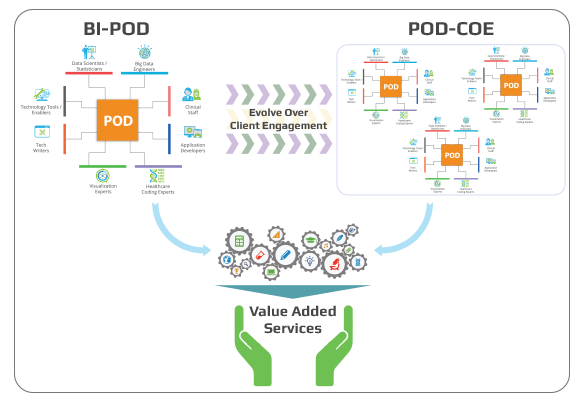 Figure 1: Business intelligence POD framework, SCIO Health Analytics, 2017
Figure 1: Business intelligence POD framework, SCIO Health Analytics, 2017
These teams would come together under a POD owner who will create the right skill/effort capacity combination for the specific deliverable at hand. In addition, members of the POD team would receive specific business intelligence training from the business intelligence solution vendor. These POD team members would collaborate in an intricate fashion through a well-designed framework and defined metadata for their roles to create the tapestry needed for the delivery of the insightful intelligence that is needed to solve the most pressing healthcare challenges.
As such, healthcare organizations could rely on business intelligence POD models to provide the multiple values and differentiated outcomes for multiple constituents, while also addressing any knowledge gaps and adding a variety of useful insights.
In such a situation, the POD leader would understand the need of the hospital. The leader would then, based on the problem statement, assign a combination of most appropriate staff members. For example, if a team was looking at readmissions among hip replacement patients, an orthopedic surgeon would be included on the team. However, if the team was addressing readmissions among heart bypass surgery patients, then a cardiologist would be on the team. These clinicians would join POD teams with additional targeted resources such as statisticians/data scientists with some primer knowledge of LACE model, reporting engineers with visualization experience for creating dashboards, coders who can read into the medical records and understand the cost. As such, teams would be developed to offer the specific capacity needed to succeed with each challenge or assignment.
It’s certainly a vision worth considering – and that’s why I am asking you to envision just how your organization could put together the teams that could support this POD model. As you think about these teams, I will be thinking about how to incorporate state of the art technology into this model. Watch for my thoughts in an upcoming blog . . .
Meanwhile, have you read part 1 of this blog titled ‘Business Intelligence and Analytics Centers of Excellence: Current Models No Longer Making the Grade’? Read now.
This article was originally published on SCIO Health Analytics and is republished here with permission.
