 Deadlines are fast approaching if you plan to submit data for the 2017 Merit-based Incentive Payment System (MIPS) performance period. Don’t wait until the last minute to submit your data. Submit early and often. The two key dates are:
Deadlines are fast approaching if you plan to submit data for the 2017 Merit-based Incentive Payment System (MIPS) performance period. Don’t wait until the last minute to submit your data. Submit early and often. The two key dates are:
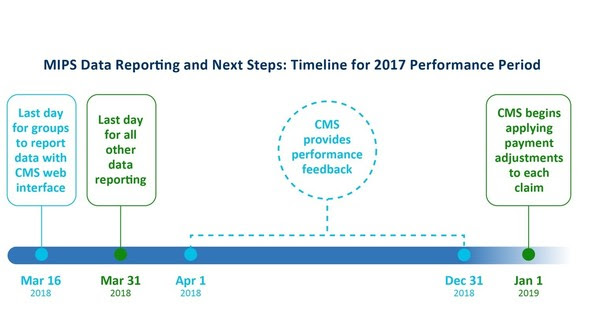
- March 16 at 8 pm Eastern time for group reporting via the CMS web interface
- March 31 for all other MIPS reporting, including via qpp.cms.gov
Now is the time to act. Here are the top 10 things you need to do and know if you are an eligible clinician. This list focuses on reporting via the qpp.cms.gov data submission feature, not on group reporting on via the CMS Web Interface and not on individual reporting on Quality measures via claims submission data.
Note: If you’re not sure if you are required to report for MIPS, enter your National Provider Identifier (NPI) in the MIPS Lookup Tool to find out whether you need to report. Additionally, if you know you are in a MIPS APM or Advanced APM, you can use the APM Lookup Tool.
1) Visit qpp.cms.gov and click on the “Sign-In” tab to use the data submission feature.
2) Check that your data are ready to submit. You can submit data for the Quality, Improvement Activities, and Advancing Care Information performance categories.
3) Have your CMS Enterprise Identity Management (EIDM) credentials ready, or get an EIDM account if you don’t have one. An EIDM account gives you a single ID to use across multiple CMS systems.
MORE EIDM TIPS: You can use your EIDM account to report for multiple NPIs associated with your EIDM. If you’ve reported for legacy programs like the Physician Quality Reporting System (PQRS), you already have an EIDM account. You can also use our EIDM Guide to get started.
4) Sign in to the Quality Payment Program data submission feature using your EIDM account.
5) Begin submitting your data early. This will give you time to familiarize yourself with the data submission feature and prepare your data.
6) The data submission feature will recognize you and connect your NPI to associated Taxpayer Identification Numbers (TINs).
7) Group practices:
- A practice can report as a group or individually for each eligible clinician in the practice. You can switch from group to individual reporting, or vice versa, at any time.
- The data submission feature will save all the data you enter for both individual eligible clinicians and a group, and CMS will use the data that results in a higher final score to calculate an individual MIPS-eligible clinician’s payment adjustment.
8) You can update your data up to the March 31 deadline. The data submission feature doesn’t have a “save” or “submit” button. Instead, it automatically updates as you enter data. You’ll see your initial scores by performance category, indicating that CMS has received your data. If your file doesn’t upload, you’ll get a message noting that issue.
9) You can submit data as often as you like. The data submission feature will help you identify any underperforming measures and any issues with your data. Starting your data entry early gives you time to resolve performance and data issues before the March 31 deadline.
10) For step-by-step instructions on how to submit MIPS data, check out this video and fact sheet.
If you are in an ACO or other APM, make sure you are working with your ACO or APM to make sure they have any patient information they need to report. Remember you need to report on Advancing Care Information measures on your own.
Questions about your participation status or MIPS data submission? Contact the Quality Payment Program Service Center by:
- Email: qpp@cms.hhs.gov
- Phone: 1-866-288-8292 (TTY: 1-877-715-6222)
