 By Abhinav Shashank, Chief Executive Officer & Co-Founder, Innovaccer
By Abhinav Shashank, Chief Executive Officer & Co-Founder, Innovaccer
Twitter: @abhinavshashank
Twitter: @innovaccer
Currently, one of the most discussed topics in the Healthcare industry is MACRA. A complex 962-page document, which is supposed to redesign the entire healthcare industry. Know all about MACRA in 6 questions.
What is MACRA?
MACRA stands for Medicare Access and CHIP Reauthorization Act. It’ll repeal the current Sustainable Growth Rate (SGR) Formula and extend CHIP for two more years. Extending CHIP for two more years (in total four years now) will help tens of millions of kids in retaining their insurance.
SGR was introduced in 1997, as a method to curb the Medicare expenditures. Under SGR the physician payments were cut if the overall expenditure was above the benchmark. This payment cut system turned out to be a major reason for significant losses incurred by physicians. Fearing payment cuts, many physicians started denying services to Medicare beneficiaries.
In 2015, ‘Doc Fix’ or MACRA was proposed, which as the name suggests fixed the unprecedented payment cuts. If it weren’t for ‘Doc Fix,’ physicians would have faced 21% payment cuts in 2015!
The Notice for Proposed Rulemaking (NPRM) was issued on 27th April 2016, and the final rule will come in November. MACRA’s full implementation will begin from 1st January 2017.
What will MACRA change/replace?
The idea behind implementing MACRA is to create something that works and is enduring. MACRA would bring changes through its unified framework called ‘Quality Payment Program’, which has been further divided into Merit-Based Incentive Payment System (MIPS) and Advanced Alternative Payment Model (APMs).
All those who will be eligible for MIPS are called Eligible Clinicians. The term has expanded from ‘Eligible Provider’ to ‘Eligible Clinicians’. It will include physicians, physician assistants, nurse practitioners, clinical nurse specialists, certified registered nurse anesthetists, and groups of such clinicians. This expansion has increased the number of people who will receive payments from Medicare. CMS might expand to Medicare part B after two years, which will include therapists, clinical social workers, clinical psychologists.
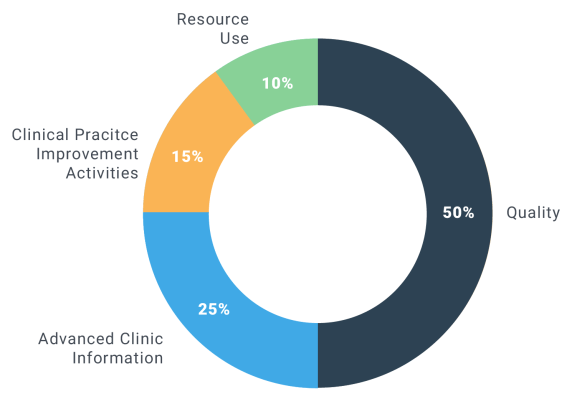
To keep health information flexible and user-centric, and bring all these changes with better care opportunities, MIPS will evaluate Eligible Clinicians on four measures namely:
- Quality Category to replace PQRS
- Resource Use category to replace Value-Based Modifier
- Advanced Care Information (ACI) to replace Meaningful Use
- Clinical Practice Improvement Activities (CPIA)
How will the four categories measure the performance?
Quality Category: Instead of reporting on nine measures, Clinicians will have the choice to pick speciality-specific measures. They can choose six measures to report to CMS that suits them the best reflecting their practice. But one of these measures must be an outcome measure or a high-priority measure and one must be a cross-cutting measure. Clinicians can also choose to report a specialty measure. Clinicians can report through Claims, Electronic Health Record (EHR), Clinical Registry, Qualified, Clinical Data Registry (QCDR) or Group practice reporting web portal.
For the year 1, Quality Category will have 50% weight in the performance scoring procedure.
Resource Use: Clinicians are not required to report for this, CMS will calculate these measures based on claims and ‘availability of sufficient volume’. To account for the differences among specialties, CMS has proposed to add 41 episode-based measures. These episode groups have potential to provide more actionable insights on measure resource use than the various cost measures.
For the year 1, Resource Use Category will have 10% weight in the performance scoring procedure.
Advancing Care Information: Clinicians can report on the measures that suit their practices the best and reflect how the EHR technology is being used for daily needs, with particular emphasis on the interoperability and information exchange. The performance score does not use threshold and allows physicians to receive partial credits on measures.
For the year 1, Advancing Care Information Category will have 25% weight in the performance scoring procedure.
Clinical Practice Improvement Activities: In this category, clinicians would be rewarded for activities that improves overall care delivery such as care coordination, beneficiary engagement, and patient safety. Clinicians can choose practices’ goal from a list of 90 plus activities. This category does not require a full year reporting. CPIA activities need to be performed for at least 90 days during the performance period.
For the year 1, CPIA Category will have 15% weight in the performance scoring procedure.
How will CMS score the categories?
CMS will use single Composite Performance Score (CPS) to factor in all the four categories to score the clinicians. Each category will have a weighted contribution in CPS. Each measure will be from 1 to 10 as compared to historical benchmarks. No points for any missed measure. Bonuses for reporting additional outcomes, patients’ experiences, appropriate use, care coordination and EHR reporting.
Calculation of Quality Scores: Consider a PQRS measure has 69% measure rate, then according to sample table in MACRA benchmark, this would equate to 8 points out of 10 possible points.
For eight measures, it would be 8 times 8 (considering all measures received equal scores), 64 out of 80 possible points, which is equal to 80%. Now multiply it by the weight of category and its percentage point will provide the weight score for CPS. 80% * 50% * 100 = 40 CPS
Calculation of Resource Use: If three measures were considered and the points were 6,7 and 8, then the weighted score would be calculated as follows:
(6+7+8)/30 * 10% * 100 = 7 CPS
Calculation of CPIA (60 possible points) and Calculation of ACI (100 possible points) are similar to Quality calculations with respective weights and possible points.
The sum of the categories will give the CPS out of 100.
What are the steps to determine the MIPS payment adjustments?
It is 6 step process to determine the MIPS payment adjustments. In the exact order:
Submission of the performance reports, Category Scoring, Calculation of CPS, Comparison with the threshold, payment adjustment determination and scaling, and payment adjustment application.
What are Advanced Alternative Payment Models?
APMs are meant for the clinicians who qualify the following:
- CMS proposes that clinicians are required to bear some risks related to monetary losses and pay to CMS when expenditures exceed the limit. Also, they might need to cut the rates and withhold payments.
- The base payments will be on quality measures comparable to those used in the MIPS quality performance category.
- Participants should use certified electronic health record (EHR) technology.
The proposed rule includes a list of models that would qualify under the terms of the proposed rule as Advanced APMs. These include:
- Comprehensive ESRD Care Model (Large Dialysis Organization arrangement)
- Medicare Shared Savings Program—Track 3
- Next Generation ACO Model
- Comprehensive Primary Care Plus (CPC+)
- Oncology Care Model Two-Sided Risk Arrangement (available in 2018)
- Medicare Shared Savings Program—Track 2
This article was originally published on Innovaccer and is republished here with permission.
