 By Rod Baird
By Rod Baird
Twitter: @rod99309
By now most of the healthcare community is familiar with the term Hospitalist. It was first coined in 1996. The earliest use of the term SNFist seems to be in a 1999 NEJM article. The name refers to a Physician or other Medical Professional who specializes in treating the residents of LTPAC institutions. Many of the clinicians who belong to the American Medical Directors Association would likely self-identify as a SNFist (although the word itself lacks any poetic qualities).
The question at hand – are there large enough numbers of Physicians, Nurse Practitioners, and Physician Assistants who practice predominantly in LTPAC to justify a special designation?
A Specialty Designation is part of a physician’s identity for Medicare Billing as opposed to a Board Certified Specialty (e.g. cardiologist). The designation becomes important when CMS compares Physicians to each other – it helps to more accurately identify patterns of practice based on a care delivery model.
This question has some immediacy following the Society of Hospital Medicine’s successful petition to CMS for a Hospitalist specialty code. There are 48,000 clinicians who self-identify as Hospitalists, how does LTPAC Medicine compare? That was a frequent question at #AMDA2016.
D-16
THEREFORE BE IT RESOLVED, that AMDA – The Society for Post-Acute and Long-Term Care Medicine initiate efforts and work with the Centers for Medicare & Medicaid Services (CMS) to seek full recognition of post-acute and long-term care medicine as a medical specialty.
Geriatric Practice Management, my organization, built a CMS data set that provides some insight into the practice of LTPAC Medicine (based in part on 2012 – 2014 Part B claims).
The following table shows three years of values for Clinicians who delivered any face-to-face encounters in the SNF/NF setting.
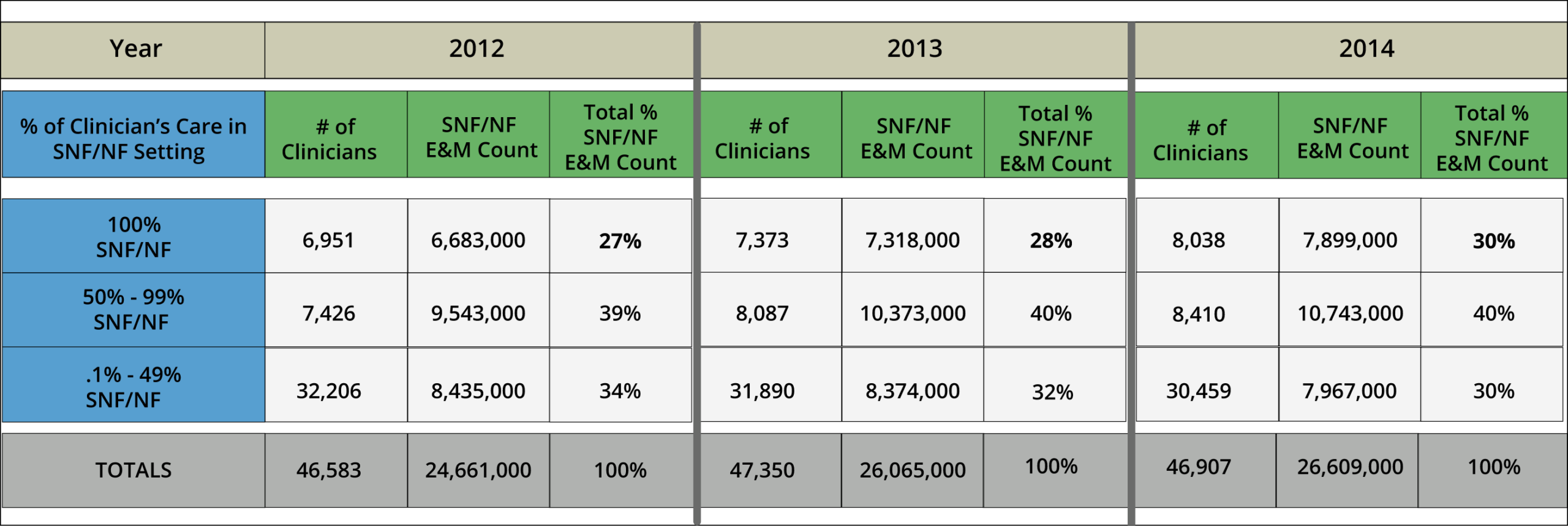
As an initial observation, the total number of Clinicians doing any SNF/NF care is steady (about 47,000). However, the amount of care (as measured by Evaluation and Management Encounters – CPT® 99304-318) is growing at a 7-8% annual rate. What is happening appears to be a trend towards a concentration of care in the hands of clinicians who spend most, or all, of their time in the nursing facility setting.
This concentration of care is something that our colleagues in practice management, and AMDA’s regulatory affairs department predicted: the complexities of the PPACA, and the associated payment rules, are likely to discourage community and hospital based clinicians from covering LTPAC. What’s gratifying is that a slightly greater number of clinicians are electing to concentrate on Nursing Home Care.
The segmentations in the table (100% Nursing Facility, 50-99%, and <50%) were chosen for clarity, and to reinforce some important points about the Meaningful Use, Value Based Purchasing, and MIPS programs.
Clinicians who are 100% SNF/NF have a very limited set of quality measures available – even a small sampling of Assisted Living Facility residents (also part of LTPAC) opens a larger set of quality measures with more favorable bench marks. Understanding that 30% of all SNF/NF care is given by clinicians who do nothing else can bolster the industry’s arguments about restrictive options.
There are endless ways to slice-up the data. If we liberalize the definition of 100% SNF/NF to include residents in Assisted Living/Adult Home locations, the new definition becomes 100% LTPAC clinicians. Their head count then increases from 8,038 to 10,472. This is probably a much better number because many LTC facilities include nursing home and assisted living beds on the same campus.
The 50% threshold is important – it’s the lower limit for accessing the Meaningful Use, and ACI (Advancing Clinical Information) EHR Hardship exemptions. When 70% of all care is delivered by clinicians who are eligible for that exemption, perhaps it’s time for CMS/ONC to rethink how they structure the EHR program to encourage the LTPAC Facilities to support those Clinicians use of technology. An exemption is much better than a penalty, but does little to advance patient care.
In the final analysis it seems apparent to us that there are a significant number of Medical Professionals who specialize in LTPAC. Does it make sense to seek a Medicare Specialty designation for billing and cost (resource use) measurement?
Up through the #AMDA2016 conference, we supported this wholeheartedly. However, during May, CMS published a whitepaper titled CMS Patient Relationship Categories and Codes. This proposal, mandated by MACRA, directs CMS to establish a methodology for associating Physicians and Practitioners with Medicare Beneficiaries. The purpose is to establish a more nuanced determination of the billing entity’s responsibility for both Resource Use and Care Episodes.
If CMS implements these Relationship Categories and Codes for billing, the use of a SNFist Specialty Billing Code will be a crude tool of minimal value. Of course, the corollary is that the physician, or their billing team, has to select a new code for each encounter/episode and include it on the bill. Does this sound like revisiting the pain of delivering ICD-10 to your claims?
In the months to come, we’ll post new insights into the Part B Claims data. If readers have specific topics they are interested in, please let us know.
About the Author: Rod Baird is founder and president of Geriatric Practice Management (GPM) and gEHRiMed. Since 1977, he’s led provider and management organizations that deliver care to Medicare/Medicaid beneficiaries. He also was chosen to be a part of the Centers for Medicare and Medicaid Services’ (CMS) Innovation Advisors Program. Originally posted on LTC Management with permission to syndicate.
