 By Leslie Athmer, MBA, Director, Product Success, SA Ignite
By Leslie Athmer, MBA, Director, Product Success, SA Ignite
Twitter: @saignite
The QPP Performance Feedback Reports for 2018 were released on July 1, 2019 and can be downloaded by logging into your QPP account. As confirmed with CMS, this report is considered your final score for the 2018 performance year. Below, I wanted to share some insights on the Feedback Reports that we have found from analyzing our customer base.
- Payment Adjustment: If you downloaded the report right when it was released, you may have noticed that there was no payment adjustment anywhere on the report and a large “PENDING” watermark. They have since been updated: the payment adjustments are now available, and the watermark removed. A perfect MIPS score yields a 1.68% adjustment which will be reflected on reimbursements in 2020. Last year, CMS continually had to update the payment adjustment amounts as they completed the targeted reviews, so we still may expect some changes to these adjustments once reviews are complete at the end of August. This adjustment is slightly lower than the CMS projection, but similar to what we saw in 2017 as well. The overall adjustment was expected to be lower due to the higher low volume threshold removing many smaller practices from eligibility. These small practices made up a large portion of penalties in 2017 which make up the base incentive amount.
- Scores: A vast majority of clinicians and TINS received full points on the PI & IA categories, which comes as no surprise. Overall, we are seeing fewer perfect scores at the TIN level as compared with 2017, which again, is no surprise with the 10% Cost weighting. Some individual clinicians did receive perfect scores, mostly because their entire Cost category was reweighted to Quality. There has been no change from last year regarding individual clinicians filing on top of the group. If the individual clinician has a higher score than the TIN, then that clinician receives an individual feedback report, and otherwise would inherit the TIN scores/feedback.
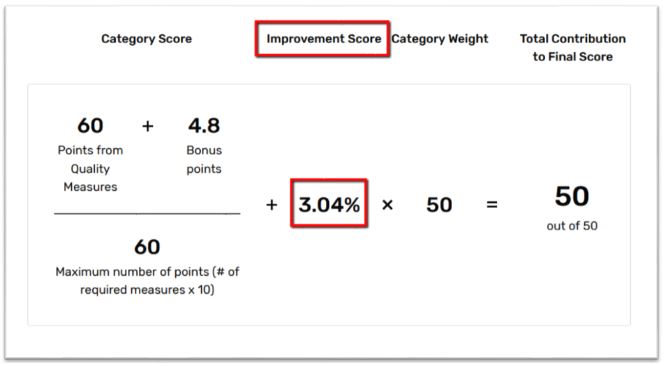
- Bonus Points: The available bonus points have helped offset some of the negative impact of the Cost category. At initial glance, it seems as though the Complex Patient Bonuses are higher than what we were seeing on the Preliminary Feedback Reports. Additionally, the bonus points for the Quality Improvement score is now reflected, which attributes up to 10 percentage points (!) to the Quality category score based on performance improvement from 2017 to 2018. You will see this figured directly into the Quality score calculation. If there was no improvement, the reference to Improvement score is not displayed anywhere on the report. The addition of up to 10 percentage points can have a huge impact and really help compensate for lower Cost scores.
- Cost: The Cost category does reflect data for the Medicare Spending Per Beneficiary (MSPB) and the Total Cost Per Capita (TPCC) measures if the minimum threshold for each measure is met. If neither of the thresholds are met, then the report displays as “N/A” for cost and the entire category gets reweighted to Quality. Just like last year, you also do not receive any feedback data for the measures if you are not meeting the thresholds. The Cost category will state “Cost data is not currently available and will NOT be assessed for payment purposes.” We were hoping to get insights on the new 2019 Cost measures on the report, since they provided insights for MSPB & TPCC on the 2017 reports, however that is not the case. Unfortunately, we still have no data points for the new 2019 Cost measures. There is, however, beneficiary level information that can be downloaded from the QPP portal on the MSPB & TPCC measures that may provide some more clinician level insights.
Hopefully the reports look as expected as compared with the preliminary reports during submission. As always, if there is a surprise or unexpected outcome on your Feedback Report, I would encourage you to file a Targeted Review with CMS to revisit the scores.
This article was originally published on SA Ignite and is republished here with permission.
