On October 1, 2015 health systems across the country transitioned to the International Classification of Diseases, 10th Revision – ICD-10. This change will enable providers to capture more details about the health status of their patients to improve patient care and public health surveillance.
CMS has been carefully monitoring the transition and is pleased to report that claims are processing normally. Generally speaking, Medicare claims take several days to be processed and, once processed, Medicare must– by law – wait two weeks before issuing a payment. Medicaid claims can take up to 30 days to be submitted and processed by states. For this reason, we will have more information on ICD-10 transition in November. .
With this in mind, CMS is continuing its vigilant monitoring process of the ICD-10 transition and can share the following metrics detailing Medicare Fee-for-Service claims from 10/1-10/27.
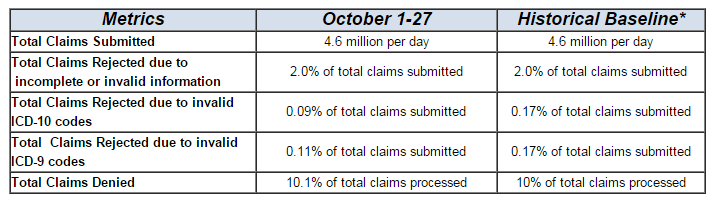
NOTE: Metrics for total ICD-9 and ICD-10 claims rejections were estimated based on end-to-end testing conducted in 2015 since CMS has not historically collected this data. Other metrics are based on historical claims submissions.
It’s important to know help remains available if you experience issues with ICD-10:
- For general ICD-10 information, we have many resources on our Road to 10 website and the ICD-10 website.
- Your first line for help for Medicare claims questions is your Medicare Administrative Contractor. They’ll offer their regular customer service support and respond quickly.
- You can contact the ICD-10 Coordination Center.
- The ICD-10 Ombudsman, Dr. Bill Rogers, can be your impartial advocate.
