By Jeff Jones, Executive Project Assistant, GroupOne Health Source Inc.
By Jeff Jones, Executive Project Assistant, GroupOne Health Source Inc.
Twitter: @GroupOne_Health
In April we published a post announcing the launch of the new risk-based primary care initiative, Comprehensive Primary Care Plus (CPC+). So what should you know before submitting your application? We’ve compiled a list of frequently asked questions about the CPC+ program and some answers to help you better understand it.
Understanding the Two Paths to the MACRA Legislation
Before we go further into the Comprehensive Primary Care Plus program, I want to make sure I touch on how the CPC+ program fits into the MACRA legislation.
As many of us now know there are two paths to the MACRA legislation. One is the Merit-based Incentive Payment System (MIPS) path and the other is the Advanced Alternative Payment Models (APMs) path.
In order to participate in the APMs path clinicians must prove “significant” participation in an Advanced Alternative Payment Model. In doing so, those clinicians will be:
- Deemed Qualified Participants (QPs)
- Receive a 5% lump sum bonus (according to their previous year’s Medicare Part B reimbursement)
- Be entirely excluded from MIPS
In this article, we’ll discuss one of the six Alternative Payment Models that have been deemed an Advanced APM by CMS for the first performance year of 2017; the Comprehensive Primary Care Plus (CPC+) payment model.
The enrollment period began on August 1, 2016 and will end on September 15, 2016. Visit the CMS portal to submit your application today.
What is the Comprehensive Primary Care Plus Program?
CPC+ is a CMS program that is a new medical home model that aims to strengthen primary care through a regionally-based multi-payer payment reform and care delivery transformation.
The new CPC+ model builds on the previous Comprehensive Primary Care program, which launched in late 2012 and will run through December 31, 2016. CPC+ integrates many lessons learned from CPC, including insights on practice readiness, the progression of care delivery redesign, actionable performance-based incentives, necessary health information technology, and claims data sharing with practices.
CPC+ will include two primary care practice tracks, both of which include care delivery redesign to ensure practices in each track have the infrastructure to deliver better care to result in a healthier patient population.
The multi-payer payment redesign will give practices greater financial resources and flexibility to make appropriate investments to improve the quality and efficiency of care, and reduce unnecessary health care utilization.
Where is CPC+ Available?
In an Aug. 1 press release CMS Deputy Administrator and Chief Medical Officer Patrick Conway, M.D., said CMS views CPC+ as the future of primary care in the United States. He noted that payers involved in the project were “committed to supporting primary care practices of all sizes.”
He specifically mentioned small, independent and rural practices. “This model allows primary care practices to focus on what they care about most — serving their patients’ needs when and how they (physicians) choose.”
CPC+ will be available in 14 regions, which were chosen based on payer interest. The selected regions include the states of:
- Arkansas
- Colorado
- Hawaii
- Michigan
- Montana
- New Jersey
- Ohio
- Oklahoma
- Oregon
- Rhode Island
- Tennessee
Also included are the North Hudson-Capital region in New York, the greater Kansas City area in Kansas and Missouri, northern Kentucky and greater Philadelphia.
What is the goal of the Comprehensive Primary Care Plus Initiative?
CPC+ will bring together CMS, commercial insurance plans, and State Medicaid agencies to provide the financial support necessary for practices to make fundamental changes in their care delivery.
CMS will enter into a Memorandum of Understanding (MOU) with selected payer partners to document a shared commitment to align on payment, data sharing, and quality metrics throughout the five year initiative of CPC+.
The goal of CPC+ is to improve the quality of care patients receive, improve patients’ health, and spend health care dollars more wisely. Practices in both tracks will make changes to the way they deliver care based upon key Comprehensive Primary Care Functions:
- Access and Continuity
- Care Management
- Comprehensiveness and Coordination
- Patient and Caregiver Engagement
- Planned Care and Population Health
How are Providers Paid with the CPC+ Program?
In order to support the delivery of comprehensive primary care, CPC+ includes three payment elements:
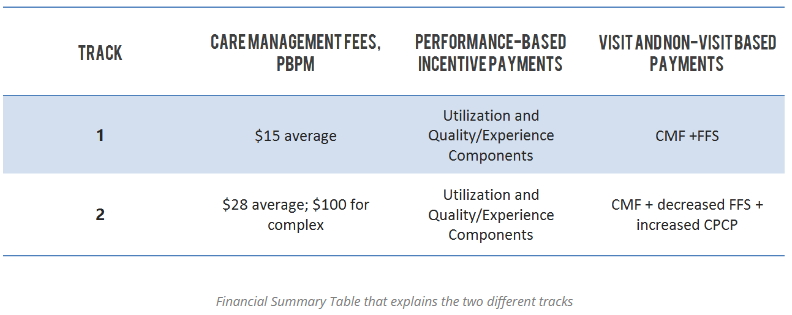
- Care Management Fee (CMF): Both tracks provide a non-visit based CMF paid Per Beneficiary Per Month (PBPM). The amount is risk-adjusted for each practice to account for the intensity of care management services required for the practice’s specific population. The Medicare FFS CMFs will be paid to the practice on a quarterly basis.
- Performance-based incentive payment: CPC+ will prospectively pay, and retrospectively reconcile, a performance-based incentive, based on how well the practice performs on patient experience measures, clinical quality measures, and utilization measures that drive total cost of care
- Payment under the Medicare Physician Fee Schedule: Track 1 continues to bill and receive payment from Medicare FFS as usual. Track 2 practices also continue to bill as usual, but the FFS payment will be reduced to account for CMS shifting a portion of Medicare FFS payments into Comprehensive Primary Care Payments (CPCP), which will be paid in a lump sum on a quarterly basis absent a claim. Given CMS’s expectations that Track 2 practices will increase the comprehensiveness of care delivered, the CPCP amounts will be larger than the FFS payment amounts they are intended to replace.
How Does Technology Support CPC+?
In order to understand and assess care quality, CMS requires practices to adopt a CPC+ ready EHR that is capable of adopting many of the following workflow changes:
- Utilizing an IT-enabled, patient-centered care planning tool
- Tracking patients over time
- Administering surveys and tracking survey status
- Linking results to care plans
- Triggering interventions based on results
What If I am Using eClinicalWorks EHR?
eClinicalWorks has signed a Memorandum of Understanding to assist practices who choose to pursue CPC+ for Track 1 or Track 2. For those looking to apply for Track 2, eClinicalWorks is on CMS’ approved vendor list and has signed the Health IT Vendor MoU which must be included with your application. eCW is also providing the following:
- Access to the care coordination and management tools your practice needs to qualify, and ongoing customer support beyond the Jan. 1, 2017, start of the CPC+ program
- APM – Advanced Alternative Payment Models webinar
- CPC+ informational presentation
For more information and/or Practice Materials, Health IT Vendor Materials, and Payer Materials, visit CMS.gov
Questions about CPC+?
Don’t forget all applications must be submitted by September 15, 2016 at 11:59 EDT. Register and submit your CPC+ application today.
This article was originally published on GroupOne Healthsource and is republished here with permission.