By Chelsea Richwine, Wes Barker, Jordan Everson, and Vaishali Patel, ONC
By Chelsea Richwine, Wes Barker, Jordan Everson, and Vaishali Patel, ONC
X: @ONC_HealthIT
The world is better off and getting better, compared to popular opinion and what’s broadcast on the news, says Hans Rosling and his co-authors, using simple, comprehensive measures, in Factfulness. Sometimes taking a step back and looking at the big picture (and the data) is important to take stock of actual progress and the necessary work to come. In that spirit, we’re kicking off a new blog series: “A Decade of Data Examined.” These posts will provide a comprehensive look at measures and metrics we’ve tracked for ten or more years to assess progress on important ONC mission activities and help chart a path forward on the work still to come. We kick off the series with a look at Patient Access to Electronic Health Information.
If you build it, will they come?
In 2013, 4 in 10 non-federal acute care hospitals and one-third of office-based physicians had adopted electronic health record (EHR) systems that enabled patients to view their online medical records. Fast forward just two years later and the proportion of EHRs with these patient access capabilities increased more than two-fold among hospitals and physicians. Today, nearly all non-federal acute care hospitals and two-thirds of office-based physicians have EHR systems that enable patients to view their electronic health information online, typically through patient portals or smartphone health apps.
The broad adoption of EHRs with patient engagement functionalities marks an important paradigm shift in health care: tens of millions of patients can now electronically access their health information including, medications, test results, visit summaries. As a result, nearly all patients visiting a hospital and many visiting their regular physician have the opportunity to become more engaged in their health and care.
This rapid transformation in providers’ capabilities to support patients’ access to their electronic health information came about through federal programs implemented from the HITECH Act, which called for the widespread adoption and “meaningful use of certified EHR technology.” Specifically, starting in 2014, eligible providers were required to adopt certified health IT with capabilities to enable patients to electronically view, download, and transmit their health information to a third party. This was largely implemented via patient portals optimized for patient engagement.
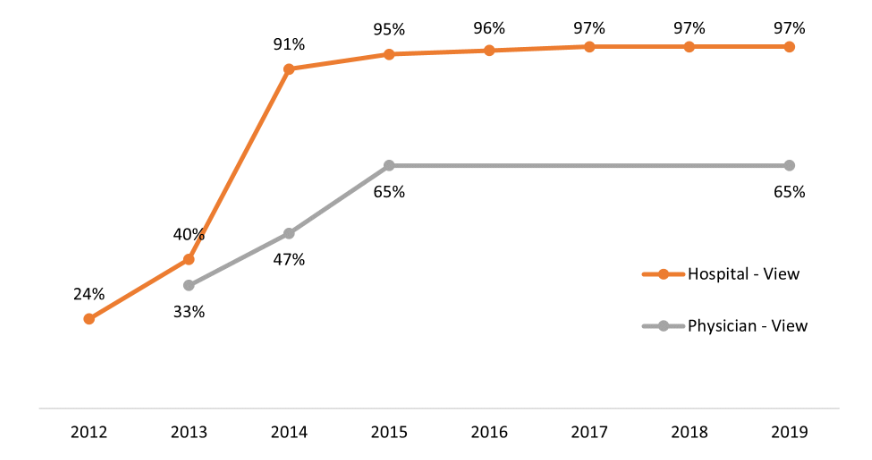
Figure 1: Hospital and physician capabilities to enable patient electronic access to health information
Source: Physician data come from the National Electronic Health Records Survey; Hospital data come from the American Hospital Association Information Technology Supplement. Notes: This figure shows the percent of office-based physicians (Physician – View) and non-federal acute care hospitals (Hospital – View) with an EHR that enables patients to view their health information in their online medical record or patient portal. In 2013 and 2014, the share of physicians with EHRs capable of enabling patients to view, download, or transmit their health information electronically is used as a proxy for ‘view’ capabilities.
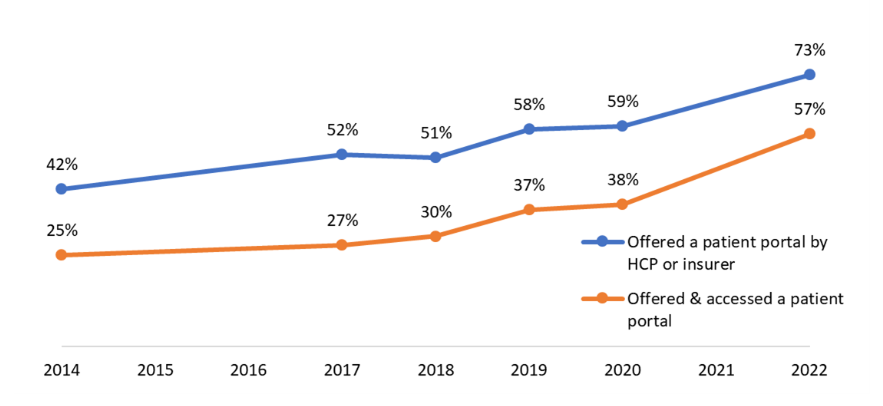
While there was rapid uptake of EHRs with capabilities to enable patient access among physicians and hospitals, individual use of this access through patient portals increased more gradually from 2014 to 2020. Usage rapidly accelerated between 2020 and 2022 when the percent of patients who accessed their patient portal jumped by 50 percent. By 2022, more than half of individuals nationally reported accessing their health information online via an app or patient portal that was offered to them by a health care provider or insurer – a more than twofold increase since 2014.
Figure 2: Individuals’ who were offered and accessed their online medical record or patient portal
Source: Health Information National Trends Survey. Notes: This figure shows the percent of individuals who reported ever being offered online access to their medical records (e.g., a patient portal) by their health care provider (HCP) or insurer and the percent individuals who reported being offered and accessing their online medical records (OMR) or patient portal at least once in that past 12 months.
This acceleration in patient access was likely driven by several factors including greater demand for accessing and sharing health information during or following telehealth visits and viewing COVID-19 test results. Additionally, patients more frequently used patient portals to message their providers (64% in 2022, up from 53% in 2018, prior to the pandemic). To support this rising demand, there was also substantial growth in health care providers offering access to patient portals and encouraging their use. The upward trend in patient access may also reflect general increases in individuals’ comfort using technology to manage their health care and track progress on health-related goals.
Furthermore, growth in patient access may also be a result of the broader shift towards app-based access to electronic health information, which can make it easier and more convenient for patients to engage with their health information online. In 2022, more than half of individuals used an app to access their health information online and these app users accessed their records more frequently compared to those who only used a web-based portal. Regulations enacted by ONC through the Cures Act Final Rule required certified health IT developers by the end of 2022 to adopt standards-based application programming interfaces (APIs) that can enable broader patient access through apps “without special effort.”
What to watch over the next decade
The types of apps used by patients to access and use their electronic health information are evolving to make it easier for individuals to manage and make use of their health data. Currently, the vast majority of app users are not leveraging emerging third-party apps that use standards-based APIs to aggregate data across multiple portals. They are largely accessing their health data via apps provided by EHR developers or health care providers to access their patient portal. It will be important to track the development and adoption of these new technologies in the coming years.
Efforts are being made to ensure patients have timely access to their health information. The recently launched Trusted Exchange and Common Agreement Framework (TEFCA) includes individual access services to ensure a core set of data will be available among networks governed by the Common Agreement to enable individuals to access and manage their health information. In 2020, 12% of individuals reported delays in receiving test results. To support patients’ right to access their electronic health information in a timely manner, ONC implemented information blocking provisions of the Cures Act, which in addition to prohibiting practices that are likely to interfere with, prevent, or discourage access, exchange, or use of electronic health information, call for the immediate release of test results to patients. Recent evidence shows that patients that immediately receive test results through their portal, rather than waiting for a call from their clinician, want to continue receiving that information immediately rather than waiting on their clinicians to deliver results. However, concerns exist about the potential negative consequences of sharing test results without the providers’ explanation, and continued monitoring will be important.
As we continue to advance and celebrate the overall growth in patient access, it is important to acknowledge and address existing inequities. Despite substantial growth in patient engagement over the past decade, several studies have documented disparities in patient access by race and ethnicity, education, income, and other socio-demographic factors. Differences in health literacy, language barriers, privacy concerns, and limited internet access are other persistent barriers to achieving widespread patient access and use of information contained in online medical records. ONC provides resources for patients on how to access their health information online using different methods and how to use, share and manage their health information. Continued monitoring is needed to inform efforts aimed at alleviating persistent barriers and ensuring patients have equitable opportunities to access their health information electronically.
In the last decade, web-based patient portals have become widely available for enabling patient access and use of electronic health information, and app-based access has made it even easier for patients to access this information. Looking forward, ONC will continue efforts to ensure patients have timely and secure access to their health information online, and that health IT developers can support novel uses of data valued by patients. Now that many patients have experienced the benefits of accessing their data for the first time, it will be important to continue to advance patient engagement capabilities that will drive patient demand for accessing and using information that can help improve health and healthcare for all.
This article was originally published on the Health IT Buzz and is syndicated here with permission.