 By Abhinav Shashank, Chief Executive Officer & Co-Founder, Innovaccer
By Abhinav Shashank, Chief Executive Officer & Co-Founder, Innovaccer
Twitter: @abhinavshashank
Twitter: @innovaccer
When the concept of a digital hospital came into the picture, the initial goal was to shift physician practices from a paper-based approach to a more flexible electronic health record systems. For widespread adoption of Health IT, the Office of the National Coordinator for Health Information Technology (ONC-HIT) was also set-up in 2004.
Although the initial focus was to enhance the efficiency of back-office operations, EHR adoption rapidly increased after the implementation of the Health Information Technology for Economic and Clinical Health (HITECH) in 2009. This digital adoption has gone through multiple iterations, and plenty has changed since EHRs first started being implemented. Now, it is time to embrace smart hospitals to maximize the use of available technology.
Trends Driving Smart Hospitals
The enactment of the Affordable Care Act and the gradual shift to value-based care brought new risk-sharing arrangements for reimbursement, where both clinical outcomes and cost savings determined part or all of an entity’s financial compensation. Technology adoption started a new culture of continuous quality improvement and connected care that allowed patient care to stretch beyond the four walls of a clinic yet maintain the quality of care outcomes. Here are a few trends in the development of smart hospitals:
1. The Boom in Healthcare Wearable Technology
A 2019 Employer Health Benefits Survey reveals that the cost of employer-sponsored insurance reached $20,576 this year. While the average employee spent $6,015 out-of-pocket, the rest was borne by employers.
In the pursuit of better health and lower out-of-pocket expenses, consumers are choosing solutions to keep track of their health metrics. Wearable tech is capable of recording data 24X7 and delivering insights based on cardiac rhythms, sleep patterns, blood pressure, exercise routines, and more. In fact, the global wearable technology market is going to surpass $32.71 billion by 2027.
Even Google acquiring Fitbit in the fitness tracking space for $2.1 billion is a testament to the fact that healthcare data is going to dominate the future and improve population health and care delivery.
2. Focus on Holistic Health Management
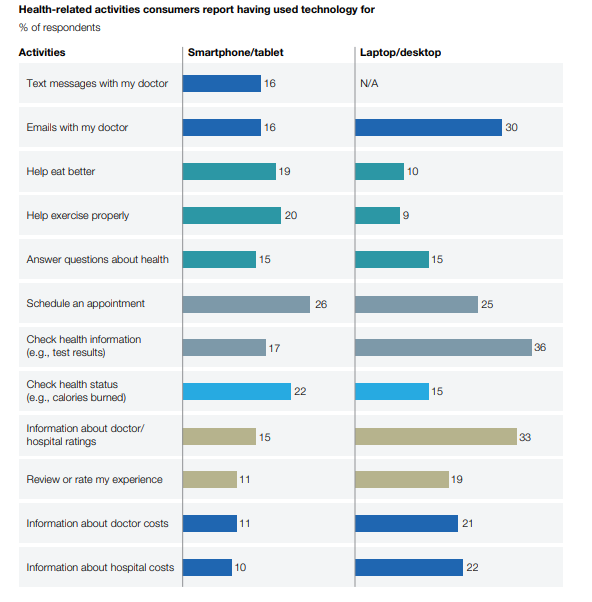
As per recent reports, US healthcare spending went beyond $3.65 trillion in 2018 and is expected to exceed $6 trillion by 2027. Therefore, the focus is to identify high-risk individuals and engage them in preventive wellness programs before they develop chronic diseases. Millennials especially are using digital technology to take charge of their wellness, introduce lifestyle changes, and stay in constant touch with their providers for preventative healthcare services.
 3. The Need for Precision at Point of Care
3. The Need for Precision at Point of Care
The need for accurate and updated patient data is another issue that smart hospitals plan to address. A leading Stanford study points out that for 7 out of 10 physicians, documenting and searching EHRs for information is a significant cause of burnout. There is no room for diagnostic or other errors at the point of care, and digital technologies such as AI and robotics are only going to empower smart hospitals and eliminate these shortcomings.
4. Focus on Chronic Care Management
Managing chronic conditions require adhering to a strict treatment plan even outside the hospital premises. Now, digital devices can be worn or simply implanted inside the body for 24×7 monitoring of specific health conditions including diabetes, high blood pressure, and cardiac ailments. Technology can help providers know if a plan of treatment is being adhered to or not, which helps contain over or under utilization of health services.
What Smart Hospitals Look Like
1. High Level Automation
Smart hospitals deploy a range of devices and mechanisms to cut down mundane activities and improve operational efficiency. RFID detection and sensing technologies are only the tip of the iceberg when it comes to creating, securing, and maintaining both patient and material records. In fact, to deal with the shortfall of nurses, a Fast Company article says that a robot named Moxi can address 30% of tasks that don’t require patient interaction. The bot can be easily programmed to run errands or deliver lab specimens.
This will free-up nurse time to invest back on patients that will certainly improve patient outcomes.
2. Focus on Patient Experiences
Smart hospitals are equipped to customize the patient experience for different levels of patient care. These stages are before, during, and after a hospital stay that can bring a drastic reduction in 30-day readmissions to boost provider efficiency and contain costs. Let’s understand with an example:
Before treatment: Smart devices like wearable technology can consistently monitor real-time patient metrics such as blood pressure and pulse rate and send updates as soon as the readings cross a threshold. The data will be automatically updated to a cloud-based EHR in real-time to alert providers. Patients can schedule a quick appointment with their provider, right from their smart devices.
During treatment: After reaching the hospital, the patient can validate their identity with device tagging, fingerprints, or facial recognition. A technology-driven interface then retrieves patient data from EHR and walks them through the next steps such as lab tests or other diagnostic procedures.
Post Treatment: The post-discharge summary and patient data can be uploaded to the cloud in real-time to generate records on the current course of treatment. A patient care app can send reminders for adherence to treatment, set guidelines for post-discharge care, and provide details on payments and insurance.
3. Consistently Gathering Data
A smart hospital runs on a data aggregation engine that never stops. Data lies at the core of a smart hospital ecosystem and is being transmitted continuously across systems to cut-down redundancy and improve quality outcomes at the point of care.
4. Movement to Outpatient Settings
Unlike traditional hospital settings, smart hospitals do not plan to offer services under one roof that can increase administration overloads and reduce efficiency. Rather, smart hospitals deliver services at smaller interconnected entities with clearly defined responsibilities. It’s important to note that preventive care and healthcare management is a critical working area for smart hospitals. For instance:
- Preventive wellness programs can be administered at clinics, gyms, and homes; based on the risk factors of an individual
- Regular medical treatments and routine minor procedures are done at ambulatory centers
- Diagnostic testing is provided at designated centers
So, in a smart hospital model, hospitals have to manage only critical activities that are impossible to be managed by smaller entities or tasks requiring meticulous coordination. Major surgeries, trauma management, chronic disease management, and other complicated conditions are a few activities that demand a higher level of medical supervision.
The Road Ahead
Fragmented care delivery poses a challenge for providers and prevents them from achieving care objectives. In a smart hospital, providers don’t have to work in silos for delivering care. Data completes the loop with care managers, patients, and other stakeholders having real-time access to patient data. This way, providers not only can improve the operational efficiency with better utilization of resources but can be better equipped to perform necessary course corrections to close the care gaps.
This article was originally published on Innovaccer and is republished here with permission.
