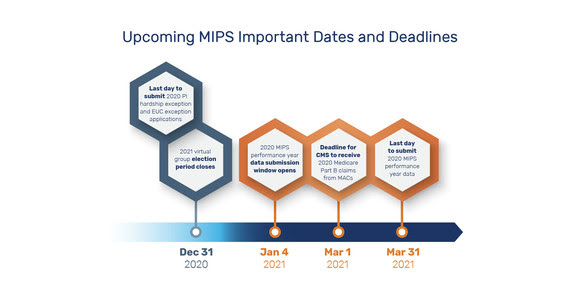
 The Centers for Medicare & Medicaid Services (CMS) (@CMSGov) would like to remind clinicians of important upcoming Merit-based Incentive Payment System (MIPS) dates and deadlines:
The Centers for Medicare & Medicaid Services (CMS) (@CMSGov) would like to remind clinicians of important upcoming Merit-based Incentive Payment System (MIPS) dates and deadlines:
- December 31 – 2020 Promoting Interoperability Hardship Exception and Extreme and Uncontrollable Circumstances Exception Applications Clinicians, groups, and virtual groups who believe they are eligible for these exceptions may apply, and if approved, will qualify for a re-weighting of one or more MIPS performance categories. CMS will notify applicants via email whether their requests are approved or denied. If approved, the exception will also be added to the QPP Participation Status Tool but may not appear in the tool until the submission window opens in 2021.
- Note: CMS has proposed for the 2020 performance year to allow Alternative Payment Model (APM) Entities to submit Extreme and Uncontrollable Circumstances applications as a result of COVID-19. For more information about the impact of COVID-19 on Quality Payment Program participation, see the Quality Payment Program COVID-19 Response webpage.
- December 31 – 2021 virtual group election period closes. Solo practitioners and groups with 10 or fewer clinicians (including at least one MIPS eligible clinician) who want to participate in MIPS as a virtual group for the 2021 performance year must submit their election to CMS.
- January 4, 2021 – 2020 MIPS performance year data submission window opens.
- March 1, 2021 – Deadline for CMS to receive 2020 claims for the Quality performance category. Claims must be received by CMS within 60 days of the end of the performance period. Deadline dates vary to submit claims to the MACs . Check with the MACs for more specific instructions.
- March 31, 2021 – 2020 MIPS performance year data submission window closes.
For More Information
To learn more, visit the QPP website and access the following resources:
Questions?
Contact the Quality Payment Program at 1-866-288-8292 or by e-mail at: QPP@cms.hhs.gov
To receive assistance more quickly, please consider calling during non-peak hours—before 10 a.m. and after 2 p.m. Eastern Time.
- Customers who are hearing impaired can dial 711 to be connected to a TRS Communications Assistant.
