Ask Joy: This Week – Align Your Efforts
Ask Joy: This Week – Align Your Efforts
Last week, I presented a Learning Lunch on how to make the most of your efforts in measuring quality outcomes. With multiple public and private incentive and accreditation programs out there, providers may find it challenging to meet the requirements of each program. Know that there are ways to streamline your efforts. One of the most common ways to align outcome measuring is by overlapping CQM and PQRS measures to meet both programs. We’ve already discussed how to do this here and here.
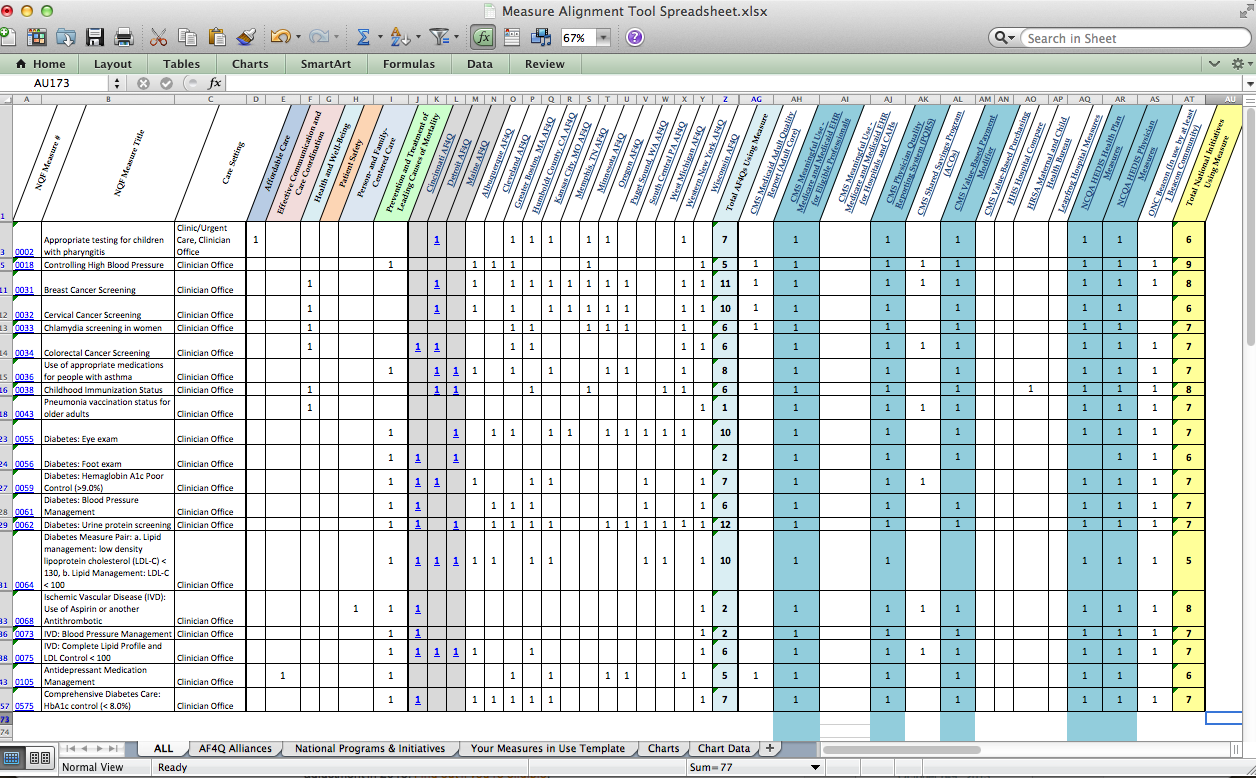
But, did you know about the Alignment Tool? The National Quality Forum (NQF) gathered insights from 16 different alliances to try to reduce the administrative burden of capturing quality data for the various programs measuring such things. Of the 179 quality measures they reviewed, I found 20 that apply to CQMs, PQRS, HEDIS, and PCMH. I’ve included a screenshot of the tool, with these 20 highlighted so you can get a quick idea if this is something that will help your practice align your efforts to gain the maximum incentives and potentially start working toward Patient Centered Medical Home (PCMH) or Accountable Care Organization (ACO) accreditation. NQF also has searchable database of these measure portfolios that allows you to compare programs and quickly access resources related to quality measurement.
Some great questions arose from our conversation. Check them out:
If aligning CQM and PQRS measure reporting, and submitting electronically on or after 1/1/2015, but attesting on the 1st quarter of 2014, will the incentive payment not come in until after CQM/PQRS measures are submitted?
That is correct. The CQM reporting period is only 90 days for 2014, but the PQRS reporting period is a full calendar year. To account for this, CMS will hold the incentive payment until the CQM/PQRS measures are submitted and reviewed. Submission of 2014 CQM/PQRS data will take place between January 1 – February 28, 2015. So, even if your Meaningful Use attestation is on the first quarter of 2014, expect payment in the first quarter of 2015.
Amongst all the Quality Programs mentioned here, which as per Joy is the most preferred one to go for, especially when you compare Effort vs Results… PQRS, PCMH or HEDIS?
My unofficial advice would be to start with the CQM/PQRS Pilot Program. Depending on how that goes for your practice, if you’re interested in taking the PCMH path, that would be the next step. Remember PCMH involves more coordination and uses Meaningful Use as a base for the program. So, master Meaningful Use first, then get started on PCMH. If you want to continue down that road, joining an ACO would come after accomplishing PCMH status.
Are patient reported measures spanning programs included in this analysis? How would those be collected/submitted?
Great question! No, patient reported measures are not included in this analysis. However, here are answers to common questions about patient reported outcomes measures (PROMs), hosted by the National Institute of Health.
CQM and PQRS have been tied to incentives. Will they ultimately be tied to payment adjustments. If so when will that occur and what are the penalties?
Yes. The payment adjustments for both CQMs and PQRS begin in 2015. PQRS penalties are tied to the 2013 reporting year, and will be a negative 1.5% of Medicare PFS reimbursements. Here is a good resource to get an idea of the full impact of PQRS incentives & penalties.
CQM penatlties begin in 2015 and will be a negative 1% of Medicare PFS reimbursements. The penalty will increase by 1% each year and cap out at 5% negative reimbursement in 2019. To avoid the 2015 penalty, EPs must meet the requirements for Meaningful Use in 2013. To avoid the 2016 penalty, EPs must meet the MU requirements in 2014, and so on.
So just to clarify, in order to satisfy my 2014 Meaningful Use CQM requirement, if I submit 9 CQMs covering 3 domains based on a 1/1/14 – 12/31/14 reporting period, I will have fulfilled my 2014 CQM and PQRS requirements?
That is correct. They have aligned PQRS measures with CQMs. Just remember to notify CMS on the CMS Registration & Attestation website that you plan to participate in the PQRS Medicare EHR Incentive Program Pilot and will be submitting your CQM & PQRS reports together in early 2015. Follow these instructions.
About the Author: Joy Rios has worked directly with multiple EHRs to develop training programs for both trainers and practice staff. She has successfully attested to Meaningful Use for multiple ambulatory practices in both Medicare and Medicaid. She also authored the Certified Professional Meaningful Use course for www.4Medapproved.com. Joy holds an MBA with a focus in sustainability. She is Health IT certified with a specialty in Workflow Redesign, holds HIPAA security certification, and is a great resource for information regarding government incentive programs.Ask Joy is a regular column on 4Medapproved HIT Answers.