 By Rose Higgins, President, North America, SCIO Health Analytics
By Rose Higgins, President, North America, SCIO Health Analytics
Twitter: @SCIOanalytics
The Medicare Share Savings Program (MSSP) enables providers to assume value-based risk on care delivery for defined populations. Based on a value-based care model that rewards healthcare organizations for improving outcomes, the Shared Savings program promotes accountability for a patient population; coordinates items and services for Medicare fee-for-service beneficiaries; and encourages investment in high quality and efficient services.
As such, organizations participating in MSSP have quite a bit of work on their plate. And, they often focus keenly on reporting quality and utilization benchmarks. But organizations need to do much more to ensure their financial house stays in order so they can continue to deliver high quality care to their patients. Indeed, to succeed financially, MSSP organizations need to optimize payment on a variety of fronts to offset any potential losses. Proficient hierarchical condition category (HCC) coding can help organizations achieve financial success, ensuring that they will get paid for the services delivered and are able to appropriately track and measure network performance. More specifically HCC coding recapture can help organizations ensure that they don’t miss revenue opportunities that they might have missed the previous year and that they proactively identify opportunities throughout the year to ensure coding accuracy. In some cases, HCC coding recapture can help organizations recapture revenue to offset any unexpected deviations from your planned ACO quality and utilization performance (potential penalties).
HCC coding recapture enables ACOs to:
- Ensure patients receive the right care based on current conditions
- Identify & reduce variation in provider coding practices
- Ensure chronic conditions are appropriately documented each year
- Develop suspect lists to identify patients & providers with likely documentation errors
- Address provider variation patterns through active outreach and dialogue
- Create a single view of coding and patient risk across all payers
HCC coding recapture is a time- and labor-intensive endeavor. Using a risk adjustment analytic solution, however, can help. In fact, one Medicare Advantage organization with 68 thousand patients used this tool to close 38% of reimbursement gaps for chronic care patients. By doing so, the organization recovered $24 million in reimbursement in just one year. Additionally, a provider group, participating in an MSSP ACO, found between $1-12M in potential revenue recapture opportunity. The organization discovered variation and opportunities to optimize coding practices across several key areas in which the organization would realize a strong return by allocating efforts to improve outcomes. What’s more, another provider organization seeking to increase visibility across populations and its 850-physician network projected that it could potentially save up to $22 million reducing variations in coding capture. (See chart below).
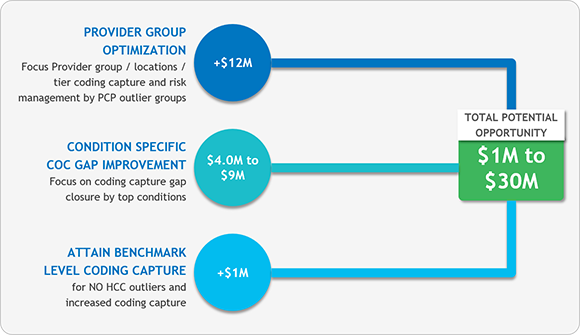
(Fig: 1) Projected opportunity for provider organization that serves 1.6 M Medicare Covered Lives
This article was originally published on SCIO HealthAnalytics and is republished here with permission.
