AMA Issues Letter and Report in an Effort to Halt ICD-10 Compliance Deadline
Last week the American Medical Association (AMA) sent a letter to the U.S. Department of Health and Human Services (HHS) Secretary Kathleen Sebelius asking that the brakes be put on the transition to ICD-10 compliance set for October 1,2014. Accompanying the letter was a new report, The Cost of Implementing ICD-10 for Physician Practices, an update to a landmark study on ICD-10 issued by Nachimson Advisors to the AMA in 2008. The report estimates the costs for providers to meet ICD-10 requirements. The report was authored by Stanley Nachimson, and Carolyn Hartley, AMA author and President of Physicians EHR.
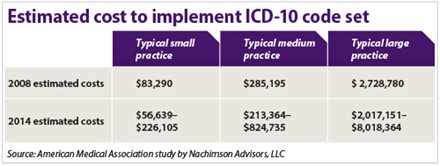
In commenting about the results of the updated report to the AMA, Carolyn Hartley said “Initial responses have been jaw-dropping and denial over the costs. However, in our analysis, we looked at ICD-10 implementation costs, plus costs to upgrade to 2014 certified EHR and ICD-10 compliant RCM systems, training on those systems, training on ICD-10, and denied reimbursements if CMS denies ICD9 claims.”
Stanley Nachimson had this to say about the report: “The purpose of this 2014 ICD-10 cost update was to use actual cost information collected over the past few years, the impact of the meaningful use requirements, and current readiness information to more accurately estimate the costs that physician practices have faced, and will face in their implementation efforts. As the study shows, a major element in the cost is for vendor/software upgrades. Practices fortunate enough to have software upgrades included as part of their contract, perhaps around one-third, will see their costs toward the lower end of our range. Our figures indicate that physician practices are facing significant cost of ICD-10 implementation, and especially the payment disruption risks. A poorly executed ICD-10 implementation effort will surely increase those risks and expose the practice to large costs in 2014 and beyond. Planning must take place now so that risks can be mitigated and practices can continue to operate effectively.”
In his AMA letter to HHS, CEO and EVP James L. Madara, MD, writes:
By itself, the implementation of ICD-10 is a massive undertaking. Yet, physicians are being asked to assume this burdensome requirement at the same time that they are being required to adopt new technology, re-engineer workflow, and reform the way they deliver care; all of which are interfering with their ability to care for patients and make investments to improve quality.
In the letter he outlines the key challenges impacting physicians as they try to comply with the new ICD-10 code set including:
- Costs associated with adoption of EHR technology to meet meaningful use requirements for the CMS EHR Incentive Program.
- Costs associated with purchasing new or upgraded EHR software that uses the ICD-10 code set.
- Costs to upgrade current practice management systems that use the ICD-10 code set.
- Financial penalties in the form of Medicare reimbursements for not meeting Meaningful Use, ePrescribing, and the Physician Quality Reporting System (PQRS) incentive programs.
- Medicare cuts stemming from the aftermath of last year’s sequestration.
Read the full 2014 AMA report here.
Read the letter to AMA here.
