
Sarianne Gruber MPH, MS
SG Healthcare Analytics LLC
Accountable Care Organizations or more commonly called ACOs plan to be the new Medicare business models for practicing medicine. What exactly is an ACO and how does it plan to measure efficiencies or inefficiencies in delivering healthcare? The premise of an ACO is to encourage healthcare providers to think of themselves as a group sharing patient care as well as financial incentives. The Medicare Gain Sharing Program, part of the new healthcare reform law, makes available the option for healthcare providers to form an ACO. There are several different options for how an ACO can organized but all must include at least primary and specialty care physicians and at least one hospital. The ACO must serve at least 5,000 Medicare beneficiaries and agree to participate in the Shared Saving Program for a minimum of three years. Financially, its providers share in any cost savings that arise from quality improvements and enhanced efficiency. The incentive plan for an ACO is simple. If the ACO is able to reduce care costs less than Medicare’s current system, then the ACO will receive a share of the savings as a bonus payment. Conversely, the plan also includes a financial penalty if an ACO misses its goal and incurs costs above the status quo.
Managing costs is one part of the ACO’s objective; the second is providing outcome evidence on the quality of healthcare provided. The ACO will be held accountable for showing improved performance on a series of 65 clinical measures and will be required to report on these quality measures for the three year agreement period. The ACO performance measures are divided in five areas of concentration: (1) patient/caregiver experience, (2) care coordination, (3) patient safety, (4) preventive health and (5) at-risk population/frail elderly health. Reviewing the list of ACO measures, 26 of the 65 requirements are also “Meaningful Use Criteria” captured with a certified EHR system. The table below lists the EHR Clinical Quality variables that can be used as a measurement source for ACO performance requirements.
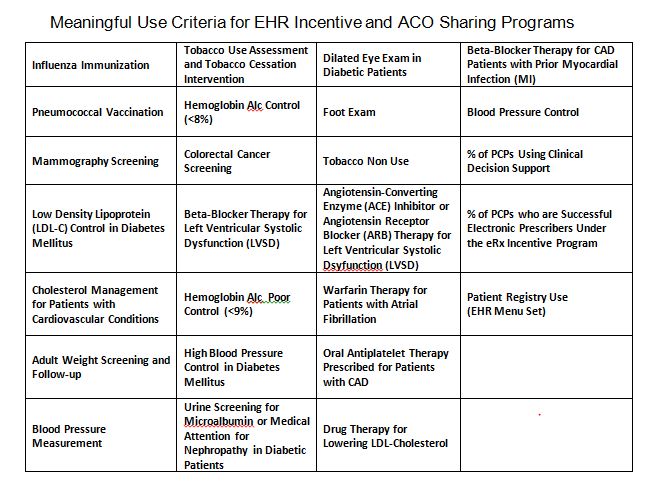
The self-reported data submission process will operate through a Group Practice Reporting Option (GPRO) web-based data collection tool, which will allow ACOs to submit clinical information from EHRs, registries and administrative data sources. The interrelationship between Meaningful Use and ACO measures brings a strong alignment between the EHR incentive program and the Shared Savings Program such that the proposed ruling will require an ACO to demonstrate that 50% of its primary care physicians are meaningful EHR users as defined by the HITECH Act. And from the “patient centeredness” perspective, the importance having the flow of patient information is critical. This can only be achieved through the exchange of electronic health information and providers who are participating in the EHR incentive program and who are developing care processes consistent with Meaningful Use.
