 By Marilyn Agbeko, Product Marketing Manager, ZirMed
By Marilyn Agbeko, Product Marketing Manager, ZirMed
Twitter: @zirmed
Ah, the good old days; perform a procedure for a patient, submit claims and get paid. To get paid more, perform more procedures. Easy math. Success lay in managing the transactions between scheduling of services and receipts of payment so that you didn’t leave money on the table.
But it was a predictable system that could be operationalized. Each transaction had a beginning and an end result that was clearly defined and as such, most could be automated. Also, you had control over most of your internal revenue drivers like your provider capacity and what you charged for your services. So, you could set up a process starting from automating patient reminders at the front end to reduce no-shows, to collecting co-pays in the office to maximize patient self-payments. The rest could be left to a good Revenue Cycle Management partner to supplement your internal systems with back end functions and payer transactions. At this point, communication was primarily between machines and systems that run in the background. Transmitting claims, reconciling deposits and remittances, identifying charge capture gaps: all are discrete transactions and can be performed by a computer.
Now though, old school rev cycle is no longer sufficient given the new fiscal reality of FFV reimbursement. Several Fee-For-Value programs are still built on the machinery that powers the Fee-For-Service infrastructure; however, you are no longer guaranteed the same amount for the same procedure. More fluid concepts like patient outcomes and satisfaction are literally affecting your money. The new revenue cycle does not start with a patient schedule and end with a remittance. It is a continuous process – a collection of smaller interactions between the people involved.
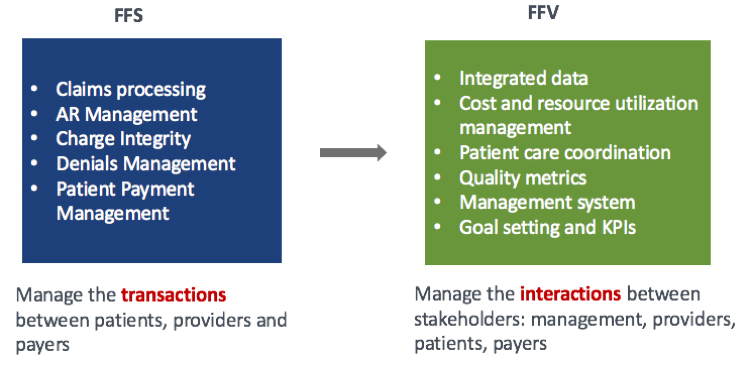
Where machine transactions are predictable and can be automated, human interaction is definitely not. However, your final reimbursement is now ultimately based on a sum total of all touch points that occur within your organization. Therefore, maximizing your reimbursement means capitalizing on each individual interaction. This requires a cultural mind shift towards high value conversations that lead to high value actions and ultimately high value outcomes.

Your job now, as a healthcare leader, is to enable these changes in behavior and slowly turn the ship. You need a management system in place that can influence providers to take proper action, and in turn influence patients. Influence means putting in place the right technology and workflows to educate and engage your providers about the business impact of their decisions, and creating the right incentives to encourage change.
What does this look like?
Dr. Smith is the CMO at General Health ACO. Her job is to ensure the success of quality programs at General Health. While looking through her Cost and Utilization data, she notices an odd trend at several of their PCP practices. Their patient populations show pretty low HCC risk scores, but incongruously high PMPM costs. Upon talking with Patrick, one of her Practice Managers, she finds that they aren’t completely capturing patient acuity with the diagnosis codes that are applied to claims, and therefore are showing lower risk scores than they should be. Dr. Smith therefore puts together training sessions for the PCPs and helps them implement a process for bringing in patients for Annual Wellness Visits. During these visits, they perform a Health Risk Assessment and identify any conditions or complications that have not been previously documented, making sure all diagnoses are accurately coded and factored into their risk score.
The conversation between Dr. Smith and Patrick leads to a conversation between Dr. Smith and the PCPs, which in turn leads to impactful conversations between the physicians and their patients. Armed with the knowledge of what to look out for and how it affects their business, physicians are able to probe deeper and surface a more holistic view of the patient than comes up in regular check-ups, if at all. Patients get better care, physicians are able to better represent the clinical acuity of their patient population, payers are able to calculate more accurate risk scores and put in place more precise cost benchmarks against which General ACO is scored.
In other words, new school revenue cycle serves as a connective tissue powering the day to day workflow of your providers and enables them to take action and maximize each interaction. The effect of this shift is better patient care and better clinical and financial outcomes.
This is not to say this is a simple task to achieve. To start, think of this question when implementing programs and new technologies: “What does stakeholder X need to get the most of their conversation with stakeholder Y?” e.g. “What do my care coordinators need to maximize the value from every patient call?”, “What do my organizational leaders need to get physicians to accept feedback on their performance?”
Answering these questions is a starting point to implementing processes and technologies that will be your first step in the 1000-mile journey to full value based reimbursement. Most of all, Don’t Panic. Unlike in A Hitchhikers Guide to the Galaxy, the answer is not simply ‘42’, but at least we know the right questions.
Stay tuned for more information on how to prepare for each stage of the VBR journey to ensure that you are set up for success.
This article was originally published on ZirMed and is republished here with permission.
