 CMS Draft 2017 Physician Fee Schedule Reaffirms that LTC Medicine Remains Misunderstood by Regulators and the AMA
CMS Draft 2017 Physician Fee Schedule Reaffirms that LTC Medicine Remains Misunderstood by Regulators and the AMA
By Rod Baird
Twitter: @rod99309
Today’s blog is focused on the inconsistent regulatory environment faced by LTPAC Medicine in the 2017 draft CMS rules in MACRA/MIPS and the Physician Fee Schedule.
These inconsistencies create economic challenges for the Medical professionals serving populations dwelling in LTC settings; equally important is the missed opportunity to incent a model of care that promotes primary care in these settings.
The Draft MACRA/MIPS regulations, for the first time, embody a clear statement from CMS which differentiates a Physician’s role in caring for a patient in a Skilled Nursing Facility (Place of Service 31), versus a LTC Nursing Facility resident (POS 32). (Copied from pg. 142 of the rule):
Patients in SNFs (POS 31) are generally shorter stay patients who are receiving continued acute medical care and rehabilitative services. While their care may be coordinated during their time in the SNF, they are then transitioned back to the community. Patients in a SNF (POS 31) require more frequent practitioner visits—often from 1 to 3 times a week. In contrast, patients in nursing facilities (NFs) (POS 32) are almost always permanent residents and generally receive their primary care services in the facility for the duration of their life. Patients in the NF (POS 32) are usually seen every 30 to 60 days unless medical necessity dictates otherwise. We believe that it would be appropriate to follow a similar policy in MIPS; therefore, we propose to exclude services billed under CPT codes 99304 through 99318 when the claim includes the POS 31 modifier from the definition of primary care services.
For readers who aren’t immersed in deciphering CMS’s unique language, the draft policy creates a clear distinction in the nature of the doctor:patient relationship in the two settings:
- POS 31 – Medical Care given to patients in Skilled Nursing Facility episodes of care is an extension of an acute care episode. In the SNF setting, Physicians and other medical professionals are analogous to hospitalists; the nature of their care is outside the definition of primary care.
- POS 32 – Individuals residing in LTC Nursing Facility beds are permanent residents, the facility is their dwelling – and the Medical Care they receive meets the definition of Primary Care. CMS expects these individuals to be served by clinicians who are applying the principals of population health management. The Physicians and Nurse Practitioners treating these individuals will have their cost/quality performance compared (benchmarked) to other ambulatory medical groups under MACRA/MIPS.
This policy distinction doesn’t correct other long standing errors in the resource use benchmarking process (LTC residents have significantly higher annual costs than their ambulatory counterparts). However, it relies on an objective measure (the presence of a Medicare Part A payment to the SNF) as a marker to distinguish between the two populations treated by the medical professionals under Medicare Part B. This lays the foundation for future methodology with a refined acuity adjustment.
Would it be too much to hope that the draft Part B Fee Schedule would align the concepts of primary care with these MIPS proposals? Apparently so.
The draft fee schedule devotes pages 143-198 to a section titled Improving Payment Accuracy for Primary Care, Care Management, and Patient-Centered Services. In my opinion, this is the clearest policy statement CMS has ever made, via the fee schedule, of its intention to transition from encounter based care to a population management model. What it fails to do is codify that LTC Nursing Facilities are locations where residents may receive these population management services.
In the fee schedule, CMS proposes to improve, and extend, the principals of Care Management via CPT® codes. In the draft 2014 Fee Schedule, CMS introduced the concept of Chronic Care Management (CCM). This was incorporated in the 2015 fee schedule as CPT® 99490 (paid at approximately $41/month for 20 or more minutes of care). When the 2015 draft schedule was published, and again in 2016, AMDA and many LTPAC Medical Groups asked if CCM applied to residents in POS 32? It wasn’t until the March of 2016 that CMS resolved this issue by issuing a FAQ (frequently asked question).
7. Can I bill CPT 99490 for CCM services provided to beneficiaries in skilled nursing facilities, nursing facilities or assisted living facilities?
If all the CCM billing requirements are met and the facility is not receiving payment for care management services (for example, the beneficiary is not in a Medicare Part A covered stay), practitioners may bill CPT 99490 for CCM services furnished to beneficiaries in skilled nursing facilities, nursing facilities or assisted living facilities. The place of service (POS) on the claim should be the billing location (i.e., where the billing practitioner would furnish a face-to-face office visit with the patient) as per #5 above.
That policy clarification opened a safe pathway for LTPAC medical groups and facilities to begin implementing population management strategies for the residents in all LTC settings.
This clarification about the applicability of CCM to POS 32 was forgotten when the draft 2017 fee schedule was published. This doesn’t mean that the principal of using Care Management in POS 32 is lost, it simply is overlooked as a Primary Care site.
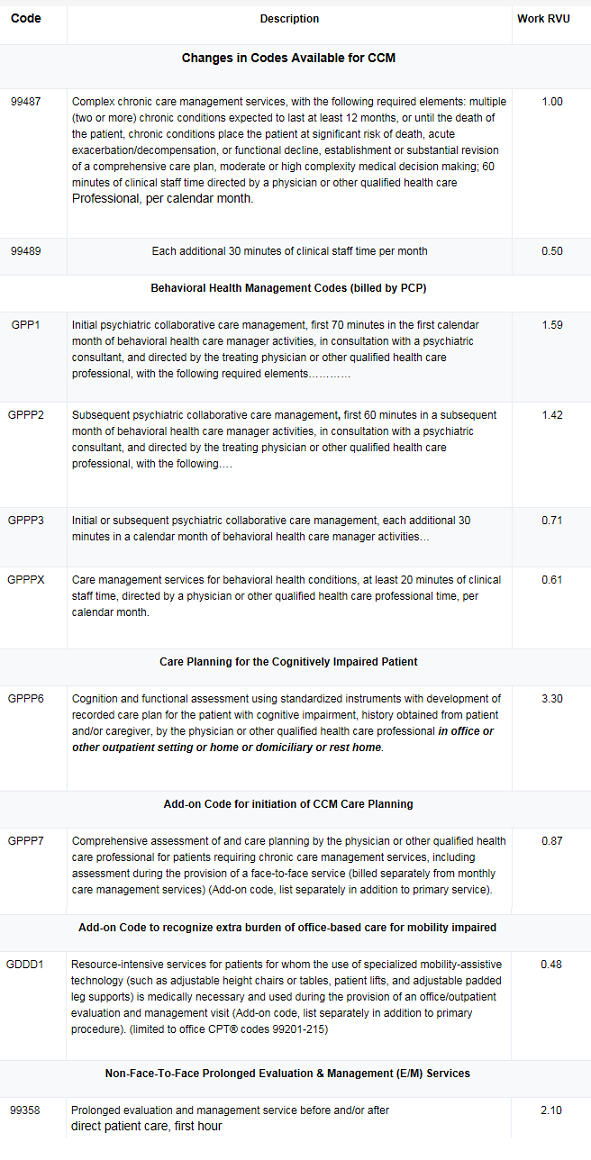
The fee schedule proposed adopting a family of care management and care coordination codes from the AMA’s CPT® panel. In several cases, the codes were still under review, and CMS elected to implement those draft definitions as HCPCS codes. To summarize the codes in the draft rule:
This blog has consistently argued that the publically insured population with the highest manageable costs are those individuals who reside in long term Nursing Facilities. These are the individuals who, under current policies, are no longer able to live independently. The nursing facility is where they live, and die, unless their death occurs during one of their frequent hospital stays. The vast majority of these individuals enter LTC nursing facility beds (Place of Service – POS32) following a Skilled Nursing Facility episode of care (POS 31).
The definitions CMS uses for these CPT® or HCPCS Codes come directly from the AMA current or proposed narrative CPT® descriptions. The AMA evaluates draft copies of CPT® codes proposed by its members – and these codes were created for Office based medicine. This isn’t to blame the AMA, their objective is to represent the interests of Physician Members – not CMS. Nowhere else but in nursing homes can the same individual, in the same physical location (room & bed) be:
- in a Part A post-acute episode of care during the day, and
- become a LTC outpatient with the updated midnight Census report.
This illogical dual identity for nursing homes didn’t exist in the earliest days of Medicare. We had separate Skilled (SNF), and Intermediate Care (ICF) nursing facilities. The Part B payment rates were lower because the SNF was cost reimbursed, which could include services to support the attending Physicians. The ICF had higher Part B Physician fees in the absence of the CMS facility payments.
When a patient exhausted their Medicare Part A coverage, they either went home or moved to an ICF Bed. This physical relocation was often disruptive and caused unnecessary suffering for the most vulnerable individuals. However, it was simple to keep track of the type of bed the individual occupied.
Patient Advocates successfully lobbied for the right of a patient to remain in familiar surroundings, and the concept of ‘dually licensed’ beds arose, this was in the 1980s. Physician CPT® coding, and reimbursement didn’t get corrected until 2006.
That’s the year when AMDA’s efforts to petition to the AMA and CMS for a new payment model bore fruit. The AMA approved new CPT® codes (99304-99318), and the CMS adopted a single uniform payment rate for those codes in POS 31 and POS 32. The logic that supported the unified payment rates for POS 31 and POS 32 was based on the elimination any extra services for physicians when SNF Part A moved from a Reasonable Cost Reimbursement payment scheme to the Prospective Payment System (RUGS rates).
It is possible to use the AMA as a vehicle to create a POS 32 specific payment model for Primary Care.
Developing a LTC Nursing Facility Care Management family of CPT® codes through the AMA would require a member organization (i.e. AMDA) to submit a validated study of the work physicians are performing that is not covered by existing CPT® codes. That is the best long-term solution, but doesn’t solve the problems LTPAC Medical Groups face today trying to implement population management. CMS also has a problem – it wants to support a switch to these new payment models for Primary Care.
Recommended Solution:
Primary Care Physicians, and Nurse Practitioners, serving LTC Nursing Facility residents are the best available clinicians to operate a ‘treat in place’ model. Those models of care can minimize avoidable hospitalizations, improve the individual’s quality of life, and conserve resources. There are nearly $2 Billion of savings (in 2005 $s) available through improving the hospitalization rates of the Medicare-Medicaid population residing in LTC nursing facilities.
Anyone interested in address this problem should register a public comment on the draft rule asking CMS to extend its policy of covering CPT® 99490 in POS 32 to the new Care Management Codes (99487, 99489, and GPPP1-GPPP7).
If LTPAC Medical Groups are financially responsible for the Resource Use of this population as Primary Care Providers, they need a full set of management tools. The opportunity to achieve the goals of the CMS triple aim far outweighs the importance of the AMA’s CPT® development process.
About the Author: Rod Baird is founder and president of Geriatric Practice Management (GPM) and gEHRiMed. Since 1977, he’s led provider and management organizations that deliver care to Medicare/Medicaid beneficiaries. He also was chosen to be a part of the Centers for Medicare and Medicaid Services’ (CMS) Innovation Advisors Program. Originally posted on LTC Management with permission to syndicate.
