By D’Arcy Gue, VP, Industry Relations, Phoenix Health Systems
By D’Arcy Gue, VP, Industry Relations, Phoenix Health Systems
Twitter: @DarcyGue
We healthcare writers spend a lot of time looking critically at federal compliance initiatives, especially the devils that may be in the details. Seriously, who even likes the unfortunate term “compliance?” Despite the hard knocks, HHS in fact has been an extraordinary trailblazer in modernizing American healthcare through information technology adoption. Sure, the for-profit private IT vendor sector has greatly contributed, but without federal privacy, security, Meaningful Use and other initially onerous programs and policies, we wouldn’t be seeing glowing reports like the following. Take a quick look and feel glad you work in healthcare.
Achievement #1: Meaningful Use Certified EHR Adoption
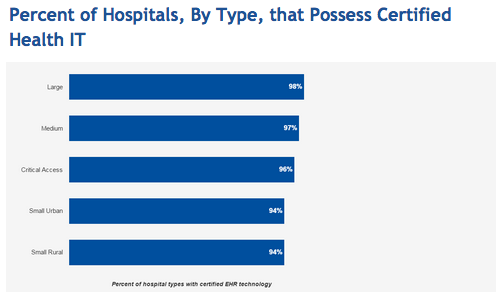
By late 2015, according to HealthIT.gov, 96 percent of all non-federal acute care hospitals possessed certified EHRs. Ninety-four percent of small rural and small urban hospitals and 96 percent of critical access hospitals had them too. An impressive 98 percent of large hospitals and 97 percent of medium hospitals had certified health IT. There is little doubt that without HHS’ Meaningful Use incentives, our healthcare system would still be languishing in the technology equivalent of the Dark Ages, desperately trying to keep up with a burgeoning patient population using a combination of disparate systems and paper-based records.
Outpatient facilities, also fueled by MU incentives, have been clipping along on the EHR road according to a new (August 2016) report by HIMSS Analytics. “Market adoption of practice management and electronic health record (EHR) solutions… is now nearing universal adoption.” The data indicates that 92 percent of hospital-owned outpatient facilities have a “live and operational” outpatient EHR solution, up from 54.5 percent in 2010. Nearly 78 percent of free standing outpatient facilities now have an EHR. If you exclude physicians close to retirement who do not feel they need EHRs, the result is near universal adoption.
Not bad for a once-onerous, fiercely resisted federal initiative. Yes, MU money was a heavy duty inducement, but of equal note is that providers could have sacrificed it. They didn’t. They knew they needed to move into an IT-oriented future.
Achievement #2: Conversion from ICD-9 to ICD-10
Bitter opposition to upgrading healthcare’s ICD diagnosis and procedure coding system forced HHS to delay industry ICD-10 adoption for years, even while most modern countries had used it for decades. Hospitals, vendors, physicians, and major healthcare associations predicted transition chaos comprised of medical errors, process disruptions, high implementation costs, and major revenue losses due to poor transactional connectivity between healthcare entities. Their objections were bolstered by the complexity of something as esoteric and seemingly inconsequential as coding; CEOs and physicians didn’t understand it and believed there were bigger concerns on their plates.
At last, HHS stood firm in 2015, requiring that providers, payors and clearinghouses go live with ICD-10 by October 1, or providers simply would not get their claims paid. In the meantime, through 2014 and 2015, HHS worked hard to provide needed information, transition methodologies and education, supported by many payors and advocacy organizations such as AHIMA and WEDI.
The result? Success. No chaos. Minimal disruption. Actually, the transition worked pretty smoothly, with minor but brief bumps within smaller providers. Compared to Canada’s tumultuous transition a few years earlier, ours went spectacularly well. WEDI reported recently that the ICD-10 implementation delays actually improved the ability of the healthcare community to perform testing and resulted in a smoother transition, even though internal process and systems changes added some costs, though fewer than feared. The impact to productivity was generally neutral for vendors and health plans, though productivity slightly decreased for providers. This appears temporary. Many provider respondents did not expect much ROI from the change. However, looking at the bigger picture, the country is now in a much better position to trade more granular disease and treatment information worldwide, to help improve national and global population health.
In a country divided, including those who criticize government effectiveness, there are strong Federal bright lights to appreciate. Our healthcare community, which has long insisted that governmental influence was unnecessary or even counter productive, has benefited from judicious intervention by HHS and even embraced it. We will have more debates in the future, but recently we’ve achieved some great wins together. This is a time when we can congratulate ourselves and HHS’ vision and leadership.
This article was originally published on Phoenix Health Systems and is republished here with permission.