 By Brian Book, President, BookZurman
By Brian Book, President, BookZurman
Twitter: @BZI_BrianBook
Interoperability of health records is certainly the buzz these days. Although there are a number of consortiums, including EHR vendors and provider organizations, diligently trying to solve this problem, there are few implemented models that achieve the goal pragmatically. And although there are barriers to interoperability that include security, network, and policy issues, the fundamental challenge is having an adequate reference implementation model for all healthcare organizations to follow. At least on the technical level there is some hope. A tool invented by Dr. Dave Carlson, and jointly developed by the Dept. of Veterans Affairs and IBM called Model Driven Health Tools (MDHT) represent that hope. It is apparent that not all organizations adhere to standards in the same way. There are several versions or interpretations of HL7, CCD, CCDA, and other standards, which does not portend interoperability in reality. What MDHT provides is a model driven approach to standard mapping for clinically useful applications and orchestration of data. What that means is that interpretations of standards like FHIR can be modeled in a uniform way so that the output is essentially a template that all developers can utilize. This reduces the variability of the interpretation and provides a more efficient tooling for subsequent applications that can consume and generate standards based data. Thus, MDHT provides an effective and uniform tool to ensure that current applications can be modified to adhere to known and accepted standards, as well as provide smarter tooling for new applications that are incorporated into the larger health IT ecosystems.
The MDHT open source project was started in 2008 with the goal of using industry standard modeling languages and tools to design and implement healthcare interoperability standards. The project was formed as part of the Open Health Tools (OHT) organization and now is an Eclipse project. From the beginning, MDHT was developed as an Eclipse plugin using UML, EMF, and OCL as the foundation. Becoming an Eclipse project is a natural fit for the technology and will open new opportunities to expand the community of developers and users for healthcare data interoperability.
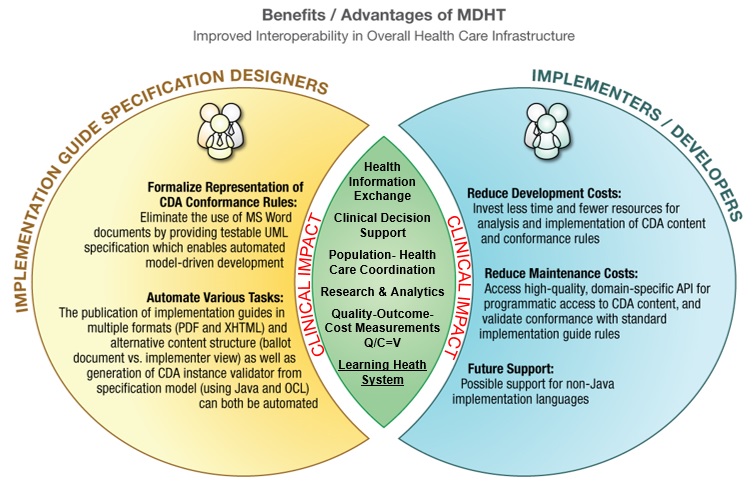 MDHT provides clear and measurable benefits to Implementation Guide Specification Designers and Implementers and Developers, but the real benefit is in its Clinical Impacts:
MDHT provides clear and measurable benefits to Implementation Guide Specification Designers and Implementers and Developers, but the real benefit is in its Clinical Impacts:
Health information exchange (HIE) and/or access to clinically relevant information is certainly a good start for impacting care. Providers and patients having such access certainly fills in the necessary information from multiple providers of care so that a more coordinated effort can occur. Specialists and primary care providers can scan all the relevant data so that duplication of effort is reduced and a broader picture of the patients’ continuum of care is available.
Clinical decision support depends on the ability to “compute” on the relevant data. This means that the data formatting needs to adhere to terminology standards, diagnostic and procedure codes with relevant context, and other contextual standards in order for there to be semantic meaning to the data. Once these semantics are available to inference and analytics engines, specific evidence based algorithms can be run in order to generate recommended care for the patient. This is the essence of “personalized care”. When you add in other relevant data points regarding the patients genomic and proteomic profiles, the computational power of guiding patients and providers based on know personal data and clinical practice guidelines, opens up a very insightful platform for improved quality of care.
Population-Health and Care Coordination also requires a similar level of semantic standard adherence in order for evidence based computations to occur across a larger population base. By querying patients at a certain age, with a specific diagnosis, based on an ICD code, and discovering that they may be non compliant on their medications or lost to follow up, allows institutions to identify these patients and take action to intervene. These are the kinds of “clinical analytics” that depend highly on standards based data.
Research and Analytics similarly depend on standards based data. The richer the semantics, or contextual meta-data, the more sophisticated algorithms that can be run in order to research complex health problems. Higher-level analytics across billions of data points among millions of patients can be revealed in order to identify trends and treatments that otherwise may not be discovered when only looking at small cohorts.
Quality and Outcome analysis is only possible if efficiently revealed using standards based data. Although manual analysis is possible and historically common, we have discovered that only with standard based clinical data elements, that represent specific quality metrics, can a efficient and reliable review of quality and outcomes be possible. And although administrative diagnostic and procedural codes are helpful, there are contextual clinical data elements that capture the true picture of the patient’s health. Without standards based data being generated or consumed by software solutions in real-time, the clinical picture is often convoluted or confused. In order for us to fully understand the value of healthcare options, we need to capture the semantically rich clinical data elements from acute care devices and electronic health systems. In order to understand value completely, we need to calculated reliable quality metrics against the cost of care. V=Q/C. The time-lines and episodes of care are part of the status and semantics that are necessarily captured electronically.
Learning Health System can be achieved by all the above standardization objectives. By being able to measure value based on quality and cost, and discovering through research and smarter analytics the best treatment plans, and cycling this knowledge back into the circle of learning, you start to see how a constant learning loop occurs. This is the capstone of standardized clinical and administrative data requirements so that we can leverage computational sciences maximally. It is also important to remember that the complexity of healthcare continues to evolve, and that the more we learn, the more we modify. This has been the history of medicine since inception. By leveraging the digital domain to assist with this evolution of learning can only help us in the long run.
To learn more about MDHT’s application or for help implementing the solution contact the BZI team.
This article was originally published on Book Zurman Inc. and is republished here with permission.
