 By Trish Rivard, CEO and Principal Consultant, Eliciting Insights
By Trish Rivard, CEO and Principal Consultant, Eliciting Insights
LinkedIn: Trish Rivard
LinkedIn: Eliciting Insights
Hospital CEOs and CFOs see a bleak financial future ahead, new law “will end up costing more than it saves.”
On July 4, 2025, President Trump signed the ‘Big Beautiful Bill Act’ into law. Under the law’s new Medicaid and Affordable Care Act marketplace policies, federal funding will decrease by $1 trillion while the uninsured population will increase by 11.8 million over the next decade.
Eliciting Insights, a healthcare market research and strategy consulting firm, surveyed thirty-two hospital executives after the bill became law to get first-hand insights on how this bill will impact the hospital industry as a whole. The respondents included CEOs, CFOs, and CMOs, and a few other C-level executives from U.S based hospital systems.
According to the survey, hospital executives believe the industry will take these top five actions to mitigate the financial strain caused by the ‘Big Beautiful Bill’:
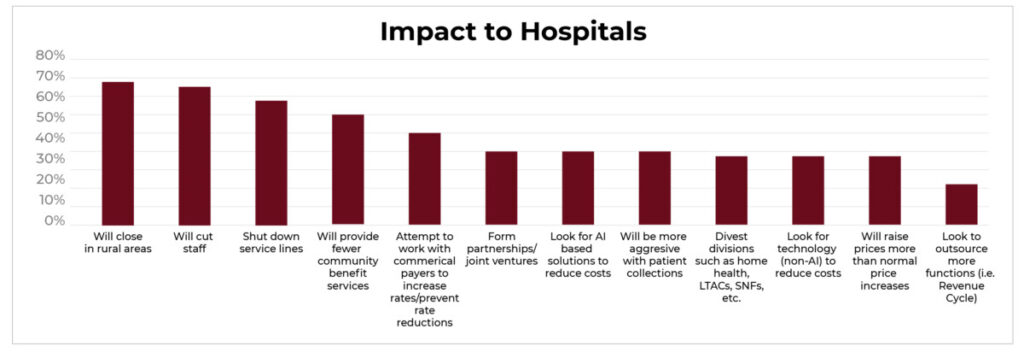
1. Rural hospitals will close.
69% of surveyed hospital executives predict rural hospitals will close because of the Medicaid funding cuts.
Small community hospitals are projected to suffer the most from this new law. Over 300 rural hospitals are at risk for closure or significant downsizing across the country because a higher percentage of their patients receive Medicaid and/or they have struggled financially the past few years.
Under the new law, $155 billion of federal Medicaid spending is getting cut from rural areas, far exceeding the allocated $50 billion to fund rural healthcare initiatives. For many hospitals, the deficit will be too large to counteract and they will be forced to close.
This will make access to healthcare extremely difficult for people needing healthcare–acute and chronic–in small communities, especially women seeking pre and postnatal care–47% of births in rural areas were Medicaid.
2. Hospitals will shut down service lines.
59% of surveyed executives anticipate hospitals will eliminate service lines.
Severe staffing shortages coupled with the increased cost of travel clinicians and the elimination of the pandemic payments led to some of the worst hospital financial performances over the past few years.
As a result, hospitals have made the difficult decision to scale back or completely eliminate service lines. These service line cuts will most likely increase when hospitals feel more financial strain from the new law’s Medicaid cuts.
3. Hospitals will provide fewer community benefit services.
53% of surveyed hospital executives predict hospitals will offer fewer community programs.
Hospitals play a crucial role in promoting wellness and health initiatives in their communities through financial assistance, health screenings, educational programs, and health fairs.
With limited resources, hospitals will face the difficult decision to discontinue these services that improve the health and wellness of their communities.
4. Hospitals will lay off staff.
66% of surveyed hospital executives predict staff cuts for the hospital industry.
With ongoing staffing shortages leading to service line cuts, it’s inconceivable that hospitals will layoff staff. However, hospitals will need to eliminate departments and staff to reduce labor costs and meet their operating budgets.
5. Healthcare providers will negotiate commercial insurance payment rates.
44% of surveyed executives think hospitals will attempt to renegotiate payments.
Medicaid accounted for 19% of spending on hospital care in 2023. To help bridge the financial gap from ‘Big Beautiful Bill’, hospital executives will need to get insurance companies at the negotiating table to request increases in payment rates or prevent rate reductions at a minimum.
Any reduction in hospital reimbursement rates or supplemental payments would further affect their financial stability.
When fewer people have health coverage, more patients won’t be able to pay their hospital bills. This leads to an increase in uncompensated care and could also mean worse health for people who lose coverage or have fewer benefits. This drives up the cost for the insured through higher insurance premiums, deductibles, and other out-of–pocket expenses.
When asked how this new law will affect patients, the surveyed hospital executives responded as follows:
- 81% predict Medicaid patients will use emergency departments as their primary care
- 78% think patients will delay treatment leading to higher levels of acuity when they come to the hospital
- 69% anticipate patients will skip preventative care
- 66% plan for longer emergency department wait times for all patients
- 44% predict patients will be turned away from non-emergent care if they are unable to pay
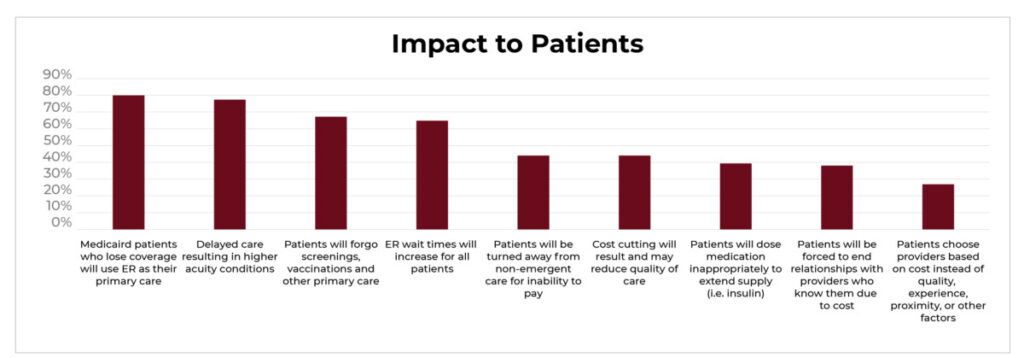
Put simply, uninsured patients will delay treatment and turn to emergency departments for all their healthcare needs, while insured patients will pay more for lower quality healthcare services.
Inevitably, the ripple effects of this massive legislation will be felt across the country. An increase in uninsured patients leads to worse health outcomes for patients and greater levels of uncompensated care for hospitals. Most hospital executives consider the new law a lose-lose situation, especially in rural and low income areas that tend to serve higher percentages of Medicaid patients.
One survey respondent said the ‘Big Beautiful Bill’ will “end up costing more than it saves.”
This article was originally published on the Eliciting Insights blog and is republished here with permission.
