By Joy Rios, Health IT Consultant at Ask Joy Health IT Consulting
Twitter: @askjoyrios
Say what you will about the pains of implementing an EHR or meeting the requirements for Meaningful Use. I’ll grant you that there are hiccups, roadblocks, stumbling points on the path to going digital. No doubt. But, you can’t deny that data doesn’t lie and when we measure data, we can manage it.
Case in point: an 11-doctor pulmonary group was scheduled to attest to Stage 2 Meaningful Use in 2014. The group’s practice manager was new to the organization and tasked with the responsibility of managing the eligible providers’ progress. She was overwhelmed and understandably nervous that the responsibility for earning $92,000 of incentive funds and avoiding a 2% penalty in 2016 was on her shoulders.
The Stage 2 requirements were a worry. The practice had just recently updated to the 2014 Edition EHR software and the patient portal had only been implemented for a month. She wasn’t sure if they could meet the patient engagement requirements and she didn’t know where they stood with the newly introduced objectives.
She asked for support through her network and found me.
Data > Information > Knowledge
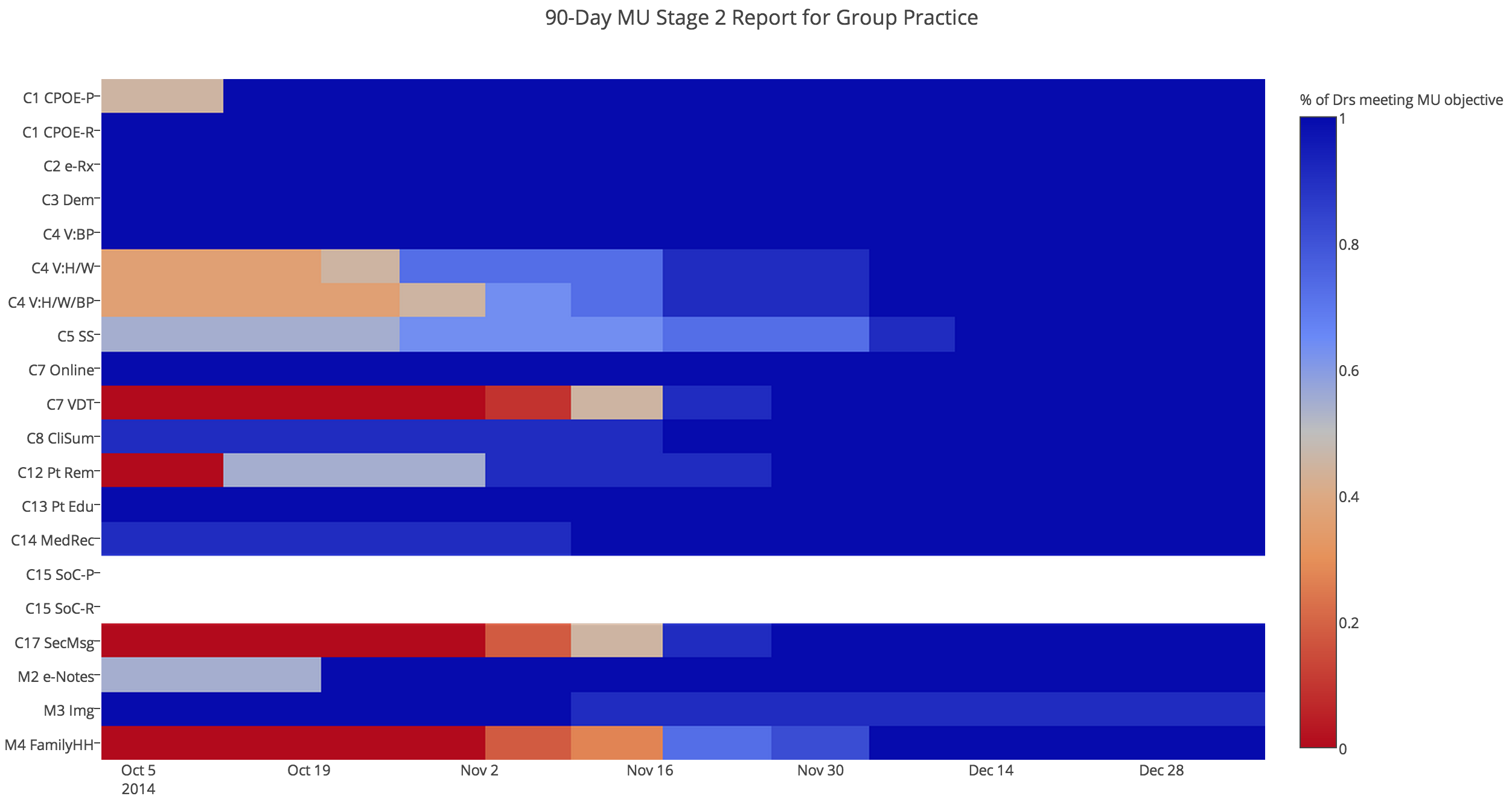
I started by getting access to her EHR and venturing to the reporting module. I found out how each provider was performing on each of the Stage 2 Meaningful Use criteria and compiled the data. In fact, you can see their starting point for yourself by looking at the left side of the below chart. (Hint: click image for better viewing)
I could see right away why the practice manager was concerned. You can see on the left side that as of October 5, none of the providers were meeting the criteria for Core 7 (VDT), Core 12 (Patient Reminders), Core 17 (Secure Messaging), or Menu 4 (Family Health History). Only half of the providers were capturing enough vitals information (Core 4) and clearly workflows needed to be reinforced for several others, including Core 1 (CPOE for medication orders), Core 5 (Smoking Status), Menu 2 (Electronic Notes).
They were able to exclude Core 15 (Transition of Care), which is why those rows are blank.
We had 90 days to turn this around.
Team Work
Armed with information, we came up with a plan. The practice manager would work with each doctor and their support staff to communicate the goals, state their status, and ensure that each person was enrolled in doing their part.
Meaningful Use is a team sport, after all.
The nurses were charged with increasing their vitals stats. The administrators made sure that reminders were sent out to patients with a specific diagnosis for preventive or follow-up care. The doctors were instructed to collect smoking statuses for more patients.
We found out that there were new features within the EHR to accommodate Stage 2, so with help from the EHR vendor, we found out how to trigger the numerators for electronic notes and for family health history. It took a couple tweaks in customization and then training on the new workflows.
With each week’s reports, we saw steady improvement. But it was important to keep the pressure on to strengthen the areas of weakness.
Getting Creative with the Portal
In November, we focused diligently on the portal. The practice has several locations, so they started a contest among them to see which office could sign up the most patients to the portal. Some locations struggled more than others, complaining of elderly patients not having access to the internet.
Ultimately, what worked best was incentivizing the patients. They purchased a bunch of $5 gift cards to Amazon and gave them out to patients AFTER they had both logged in to the portal to view, download, or transmit their health record AND sent a secure message to the doctor.
They even told patients what to say:
Dear [Provider], I was able to see my health record through the portal. Now I know where I can send you messages directly if I have questions. Thanks, [Patient]
This step alone addressed the tougher patient engagement objectives and by mid-November, we started seeing drastic improvements in the VDT and Secure Messaging stats.
The First Big Win
Around the same time, we got the first provider to meet ALL of the percentage-based requirements. It took some targeted attention to improve specific workflows, but once the first doctor demonstrated that it could be done, the others followed right behind him. By the end of November, more than half the providers were hitting the marks; and by the second week of December, all of them were.
Their main focus on closing out the year was to keep up the good work.
Non-Percentage Based Objectives
Some Meaningful Use requirements are not numerator/denominator based and require a Yes/No response. For example, were clinical decision support rules in place and did at least 5 of them related to the chosen Clinical Quality measures? Did each provider generate a patient list for a specific diagnosis for the purpose of sending reminders, outreach, or research? Was a Security Risk Analysis performed and security updates implemented to correct any identified deficiencies? Yes, yes, and yes.
Lessons Learned
1. It sure helps to have engaged team members. The practice manager served as the messenger – communicating where improvements were needed. The doctors were responsive to looking at their data, comparing it with their peers, and then making concerted efforts to improve. The office staff were all willing to step up their game when they understood the mission of engaging patients. The EHR vendor was helpful with setting up the appropriate settings and customizing the EHR when needed.
2. What gets measured gets managed. Sticking our heads in the sand and hoping Meaningful Use would take care of itself simply would not have worked. We needed to know where improvements could be made and the only way to do that was to look at the data often and respond to it.