 From the Hayes Healthcare Leaders Blog Series (@HayesManagement)
From the Hayes Healthcare Leaders Blog Series (@HayesManagement)
By Robert F. Bacon, Vice President and Billing Compliance Officer, Penn Medicine
The provider community has been begging for documentation reform for over 20 years, and there is no question that simplifying the complex requirements of clinical documentation is necessary. Unfortunately, the recent release of the proposed changes from CMS surrounding evaluation and management (E/M) is not the answer. The benefits of the modest reduction in documentation requirements are more than offset by the devastating impact the changes will have operationally, clinically, and financially.
The CMS proposed changes to the Medicare Physician Fee Schedule affects the 99201 thru 99215 Office and Outpatient Visit codes and provides a new time-based reporting option. Instead of having to document that more than 50 percent of the visit was face-to-face interaction, physicians could select a code based on the total length of the visit, without regard to how much of the time was direct patient contact.
The proposal, which would go into effect January 1, 2019 if approved, also simplifies the history and examination pieces of the three-component system for determining office visit codes, and allows physicians to select their level of service for both new and established patients using only the medical decision-making component.
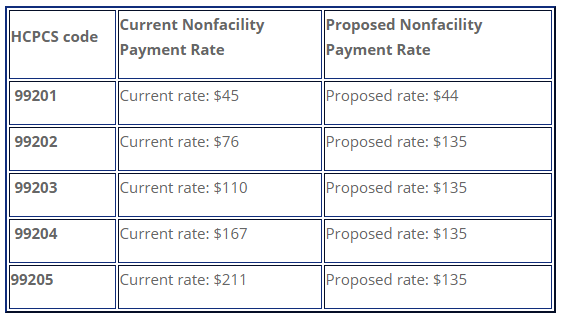
The biggest change alters the current five-level payment plan for new patients (99201-99205) and established patients (99211-99215) from five levels to two, as shown below.
However, the proposed change would not affect performance and documentation requirements for other E/M services such as emergency department or inpatient hospital visits.
While many in the industry are hailing the changes as a much-needed first step down the road to documentation simplification, the proposal may actually represent a stumble into disaster for providers, organizations and patients. Key stakeholders are being asked for their input on the proposal before September 10, and as they prepare their comment letters, I would suggest they review the following – potentially devastating – unintended consequences and assess how the changes would impact their organizations and patients.
Dual documentation requirements
The proposed changes affect only CMS and Medicare claims and would not apply to medical assistance, commercial insurers and other payers. The changes do not align with the Current Procedural Terminology (CPT) 4th edition code set, which is maintained by the American Medical Association through the CPT Editorial Panel and includes specific definitions for every service Level 1 through 5. The existing and proposed CPT codes do not correlate at all when it comes to time-based billing.
This means the codes would have to be reported as currently required for Levels 1 through 5 for new or established patients, but for Medicare claims would be submitted under the proposed rule to one of two reimbursement levels. For example, if you submit a claim as Level 4, but you’re billing a Level 4 new patient to medical assistance or a commercial payer, the limited documentation allowed for Medicare under the proposed rule would not support that same service for a non-Medicare payer.
The argument being put forth is that the commercial insurance payers will follow the CMS lead and adopt similar documentation guidelines. However, if past is prologue, that won’t be the case. There are many examples of payers choosing not to follow suit with the CMS, such as the “two-midnight” rule, which was used to determine inpatient medical necessity and was only adopted by CMS. And there is no way non-CMS payers would ever make these types of major changes by January 1, 2019.
The alternative is to implement two separate documentation guidelines: one for Medicare and another for non-Medicare payers. The concept of having two different documentation standards is completely devoid of any operational feasibility and is simply not a realistic option.
Clinical shortcomings
Documentation that is limited to “time only” – as permitted by the new rules – is certainly not going to provide a complete clinical picture of the patient. The spirit of the medical record should enable caregivers to coordinate and communicate with one another. Documentation limited to total time spent does not fulfill the purpose of communicating pertinent clinical facts about the patient to other caregivers.
Moreover, caregivers need to understand the thinking, assessment and treatment plans of previous providers when conducting follow-up examinations. How is that possible with a medical record that includes only the length of time spent, with no diagnostic notes? Why would a provider want to have a record that does not reflect the patient’s history – at least with respect to the history of the present illness? This is the only way to understand the severity of symptoms and the prescribed treatment plan to mitigate them. Medical records that don’t minimally reflect provider observations and comments is completely wrong, and is not in the spirit of documenting clinical care. A true medical record needs to “tell the story about the patient”.
Lack of budget neutrality
Any organization that has performed a financial sensitivity analysis has seen the significant loss of revenue the proposed rule would cause. CMS is asserting that the proposal is “revenue neutral” since payments for Level 2 and 3 are going up, while those for Levels 4 and 5 are going down.
The fallacy in that argument is that claims across all practice areas are not represented by a typical bell curve. For primary and family care, that may be the case, but in many other areas, the distribution is skewed to the right to the Level 4 and 5 categories reflecting a high level of medically necessary care. For academic medical centers, the odds of their claims being skewed to the right are extremely high since they rarely deal with primary care. You are not likely to see a bell curve in oncology, cardiology, or nephrology, for example. Clinicians in these areas are providing high-level care to very sick patients. The claims distribution for these specialties are all skewed to the Level 4 and 5 codes, so the increased payments from Levels 2 and 3 will not come close to offsetting the reduction in Level 4 and 5 payments.
Modifier 25 revenue reduction
Many people are focusing on the E/M changes but are not looking at the severe financial implications of the proposed change to Modifier 25, which makes E/M services subject to Multiple Procedure Payment Reduction (MPPR) discounting rules – an important nugget of information tucked into the 1,472-page document.
The proposal stipulates that when a clinician performs an E/M service in conjunction with a procedure and appends a Modifier 25 to the E/M, the E/M will automatically be discounted by 50 percent. Discounting may make some sense when the clinician is evaluating a single body part or organ system, since there is an element of evaluation and management associated with every procedure. However, when the clinician is performing a multi-system physical examination, represented in part by multiple diagnoses codes, with one or more of those codes associated with a performed procedure, and the other codes related to other body areas or organ systems, the E/M should not be discounted. A good example of this would be an emergency room patient who has been in automobile accident requiring a multi-system exam who also has one procedure performed.
The negative financial impact of MPPR discounting for the use of Modifier 25 in conjunction with procedures is simple to calculate: take all the revenue for Medicare services that include a Modifier 25 and divide it in half. The adverse financial ramifications attributable to this major change could potentially be devastating for many organizations.
Medical legal ramifications
Reducing the documentation standard to the level that the proposed rule allows can also expose the organization to significant legal ramifications. If documentation is limited to time spent, with very little content – as will be permitted under the new rule – organizations will be at risk from a medical legal perspective.
When organizations are defending malpractice cases, the core defense is based on the provider notes in the medical record. Without those notes, defending an action becomes nearly impossible. Compounding the problem is the fact that those cases can come up two or three years down the road – or even 20 years if the action involves a child. Omitting pertinent clinical information from the medical record due to a lack of legally required documentation opens the door for plaintiffs to sue based on claims that can’t be easily defended by providers.
Need for continued auditing
One thing is clear: even if this proposal is approved, the need for vigilant auditing will remain. Government and third-party auditors are not going away. There will still be audits for reporting quality measures and payments for all E/M codes, including the simplified ones. Penalties and payer reimbursements for false or incorrect coding will still exist, so the focus on accurate coding must remain a staple of your compliance program.
There’s absolutely no question that some revision is needed when it comes to documentation revision. But this proposal is a blanket change taking place overnight, with little time to prepare and without due consideration of the negative impact of any unintended consequences:
- The need for a dual reporting structure
- Insufficient patient information on medical records
- Lack of budget neutrality
- Massive revenue loss due to global discounting of Modifier 25
- Compromised defense in the event of medical legal action
The negative consequences far outweigh the benefits associated with the minor reduction in documentation this proposal offers.
We need to ease the documentation burden on clinicians, but there needs to be a better solution than the current proposal. It’s critically important that organizations submit their comments to CMS before the September 10th deadline to address the issues surrounding clinical care, operations and finance. Time is running out, so those of us in the medical community who will suffer from the consequences of these changes must act now.
Read the July 12 CMS announcement.
View the CMS proposed fee schedule.
For more blog posts from healthcare’s greatest thought leaders, check out our Healthcare Thought Leadership blog series.
This article was originally published on Hayes Management Consulting and is republished here with permission.
