 By Andy Slavitt, Acting CMS Administrator
By Andy Slavitt, Acting CMS Administrator
Twitter: @aslavitt
Twitter: @CMSgov
It was early 2015 and we had just gotten through a second successful season with HealthCare.gov, the turnaround that originally brought me into government, when the articles and letters started flying on our next big implementation – one that would affect nearly every physician and hospital in the country. And, anxiety levels were high.
On October 1, 2015, the U.S. health care system transitioned the way patient visits are coded from ICD-9 to the next version ICD-10, a system which sets the stage for meaningful improvements in public health. If people know about ICD-10 at all – and chances are they don’t – it’s probably from press reports about the more colorful diagnostic codes like “other contact with shark” or “burn due to water-skis on fire, subsequent encounter.” More seriously, for people in the health care industry, it was being compared to Y2K, a transition with the potential to create chaos in the health care system.
One representative from the physician community told me that he was concerned that half of physicians in the country wouldn’t be ready by the October 1 date. The thought of physicians in small, rural practices unable to run their practices had my complete attention. It also brought home that we are responsible for more and increasingly complex implementations – from HealthCare.gov to ICD-10 to new physician payment systems.
As I look to the future, great implementation is even more central to life at CMS.
In my time in D.C., I’ve come to see our role as implementing policies in a way that bring them to the kitchen table of the American family and to the clinics and facilities where they receive care. Implementation in this context is a vital responsibility. And there are millions of Americans that count on us to do it well: the senior filling his prescription; the trustee of the community hospital; the parents of a child with disabilities in need of home resources; the doctor who drives for miles to take care of her patients in several rural communities.
Implementation Success: 4 Lessons
It was clear that CMS had an enormous opportunity – after everything we learned from HealthCare.gov – to take the lead in smoothly implementing this new policy. The ICD-10 implementation had all the hallmarks of how CMS could drive a successful implementation and aim for excellence. The approach we took, which has become our doctrine for getting things done, had four major elements:
Lesson 1: Be Customer Focused
We believe we must always start from the perspective of the real-world needs of the people who live with the results of our implementation at the center of our work. And in the case of ICD-10, listening and learning about the issues small physician practices were facing helped us understand their resource and technical assistance needs, as well as their concerns over claims payment and cash flow.
In response, we launched “The Road to 10” aimed specifically at smaller physician practices with primers for clinical documentation, clinical scenarios, and other specialty-specific resources to help with implementation. CMS also released provider training videos that offered helpful ICD-10 implementation tips and a wealth of other material on CMS.gov/icd10. Finally, Medicare offered an unprecedented level of external testing with its three periods of voluntary end-to-end testing for physicians and other clinicians.
Lesson 2: Be Highly Collaborative
Because health care is still fragmented, CMS can’t work alone in implementing major changes. If it wasn’t for our close partnerships with the American Medical Association (AMA), the American Hospital Association, the American Health Information Management Association, state medical societies, physicians and other clinicians, billing agencies, equipment suppliers, and a variety of stakeholders, the ICD-10 implementation would not have gone as smoothly as it did. Because we listened to and collaborated with our partners, we were able to address concerns and multiply our ability to get resources to physicians. Several physician groups went from being very concerned about our approach to leading the charge on implementation. As AMA said, “We appreciate that CMS is adopting policies to ease the transition to ICD-10 in response to physicians’ concerns that inadvertent coding errors or system glitches during the transition to ICD-10 may result in audits, claims denials, and penalties under various Medicare reporting programs.”
Lesson 3: Be Responsive and Accountable
At CMS, we recognize that challenges happen and our efforts must be to anticipate them, make them visible, and be accountable for solving them. In the case of ICD-10, the potential for challenges weren’t only in our own systems, but in the systems of any physician office, hospital, or state Medicaid plan. At the suggestion of physician groups, we named an ICD-10 Ombudsman. Just as importantly, we committed to a three-business-day turnaround for every question or concern that came in from a provider. In the first month of implementation, we received approximately 1,000 inquiries and responded to 100 percent of them within three business days. We will never achieve perfection, but we will be visible and hold ourselves accountable for solving problems.
Lesson 4: Be Driven by Metrics
It’s not glamorous, but daily spreadsheets and scorecards keep complex implementations on track. Once we hit October 1, there were critical metrics to track. If doctors were sending us fewer claims, more claims than usual were denied, or a particular state was having trouble processing Medicaid claims, we needed to know as soon as possible.
Rather than waiting for the phone to ring, the CMS team created a scorecard and heat map to locate and track issues as they occurred. We launched an ICD-10 Coordination Center to handle any issues as they arose. A few days after ICD-10 launched, I received a call from a large physician organization representative asking me how things were going. I pulled out a version of the table below and read him the data. “This really is a new CMS,” he told me.
Final 2015 ICD-10 Claims Dashboard Medicare Fee-for-Service Metrics
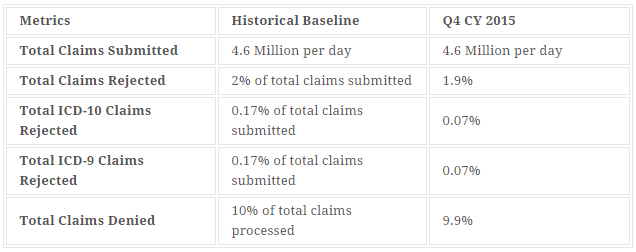 *NOTE: Metrics for total ICD-9 and ICD-10 claims rejections were estimated based on end-to-end testing conducted in 2015 since CMS has not historically collected this data. Other metrics are based on historical claims submissions.
*NOTE: Metrics for total ICD-9 and ICD-10 claims rejections were estimated based on end-to-end testing conducted in 2015 since CMS has not historically collected this data. Other metrics are based on historical claims submissions.
Moving Forward
For thousands of physicians and other clinicians around the country, the change to ICD-10 was a big undertaking, requiring time, planning, and a period of adjustment. But on October 1, proper execution and good implementation made all the difference. On the big day, the ICD-10 Coordination Center was packed, and the CMS teams and our partners were geared up and ready to make sure that any burden on physicians could be minimized and concerns quickly addressed.
With preparation, planning, a focus on the customer, collaboration, clear accountability, and metrics, the dire Y2K fears didn’t come to pass. Instead, ICD-10 became like what actually occurred on Y2K, an implementation and transition most people never heard about.
With good implementations, we never declare victory and are still at the ready to continually improve. For those who still need help, CMS continues to provide technical support and respond to inquiries. For more information, visit this website.
The magnitude of CMS’s big, complex implementations have accelerated in recent years. And over the next several years, we will be a part of implementing big and important changes that spend our health care dollars more wisely and keep people healthier – from how we pay for care to collecting and publishing data on how care is paid for to building consumer websites evaluating nursing homes to protecting beneficiary privacy and security. Because these changes impact consumers and physicians and other clinicians’ daily lives, CMS is responsible to the American people to make health care work better for the consumer and better on the front lines of health care.
This article was originally published on The CMS Blog and is republished here with permission.
